The Impact of Risk Factors on the Diastolic Dysfunction in Patients with Hypertension
Knezevic B*, Music L, Batricevic G, Bulatovic N, Nenezic A, Vujovic J, Dragovic I, Raonic M, Orlandic O, Opivoda M
DOI10.21767/2471-9897.1000013
Knezevic B*, Music L, Batricevic G, Bulatovic N, Nenezic A, Vujovic J, Dragovic I, Raonic M, Orlandic O and Popivoda M
Center of Cardiology, Clinical Center of Montenegro, Montenegro
- *Corresponding Author:
- Knezevic B
Center of Cardiology
Clinical Center of Montenegro
Ljubljanska bb-81000, Podgorica
Montenegro
Tel: 38269018160
E-mail: cicacg@t-com.me
Received date: November 20, 2016; Accepted date: December 13, 2016; Published date: December 23, 2016
Citation: Knezevic B, Music L, Batricevic G, Bulatovic N, Nenezic A, et al. The Impact of Risk Factors on the Diastolic Dysfunction in Patients with Hypertension. 2016. 2:2. doi: 10.21767/2471-9897.1000013
Copyright: © 2016 Knezevic B, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Abstract
Background: Hypertension (HTA) is often associated with other risk factors that play a role in etiology of HTA, or who may have a role in early heart damage such as diastolic dysfunction (DD).
Methods and Patients: The study included 419 patients with HTA. Patients were examined clinical, laboratory and echo cardiographic (ECHO): M-mode two-dimensional, pulsed and tissue Doppler.
Results: We found that number of HTA patients with EF<0.45 was 31 (7.4%), and number of HTA patients with diastolic dysfunction (DD) of 1 stage was 147 (35.1%). Number of HTA patients with >8 E/Ea and <15 was 112 (26.7%) and with E/Ea>15 was 15 (3.6%). The number of patients with DD was significantly higher when they had a BMI>25 kg/m² than when they had a BMI<25 kg/m² (p<0.025). The HTA patients with DD were significantly older (62.14 years vs. 52.57 years, p<0.001). The difference was significant between the HTA patients with DD age 40-49 years and age 50-59 years, between age 40-49 and age 60-69 years (p<0.001, p<0.033 respectively). The differences also exist between the number HTA patients with DD age 50-59 years and age 60-69 years (p<0.005). The differences exist between HTA patients with DD of the duration of HTA of 0-5 years and with more than 10 years of duration of HTA (p<0.018). The HTA patients with a higher level of maximum systolic BP had significantly frequently DD (190.66 vs. 183.27, p<0.005). In a multivariate analysis of paramount influence on DD were age (p=0.001), higher level of maximum systolic BP (p=0.006).
Conclusion: Left ventricular DD in hypertensive patients could be prevented if the risk factors such as obesity and maximum height of systolic BP could be controlled so to be within normal limits.
Keywords
Echocardiography; Diastolic dysfunction; Hypertension; Obesity; Age
Introduction
Hypertension (HTA) is a global worldwide problem and is at the basis of many, primarily cardiac disease. The first changes that hypertension causes on the heart are structural and geometric adaptation changes [1].
These changes cause dilatation and/or hypertrophy of the left ventricle (LV), that is remodelling LV, and they are accompanied by differences in cardiac function and hemodynamics [2]. Compensatory mechanism for hemodynamic load is the increase in mass due to the hypertrophy of existing myocytes rather than hyperplasia as a result of increase in myocyte width for parallel extensions sarcomeres which results in an increase in wall thickness [3]. In hypertension, the extracellular space is the site of an abnormal accumulation of fibrillar collagen and this progressive interstitial and perivascular fibrosis accounts for abnormal myocardial stiffness and ultimately ventricular dysfunction and is likely a result of cardiac fibroblast growth and enhanced collagen synthesis [4].
In addition to systolic function in myocardial work diastolic function is significant also, that is, the ability of chambers to fill with blood at low atrial pressure. Non-invasive measurement of diastolic function is traditionally Doppler echocardiographic measurement of mitral flow that reflects pressure gradient between the LA and LV, so that the trans mitral velocity direct reflection of the LA pressure (preload) and inversely and independently related to LV relaxation [5]. Katz described the importance of relaxation for filling LV, thus that LV not fill passively but to play a role of suction pumps [6]. This is why being tested and studied diastolic LV dysfunction in HTA, which can exist without systolic dysfunction [7].
When there is an impaired relaxation it leads to reduction of the E wave velocity and increase the speed of ‘A’ wave in order to maintain normal LV volume and cardiac output [8]. E/A ratio are considered to be commoner parameter which can get an insight of diastolic function, which is related to the filling pressure [9].
Using the Doppler principle of high amplitude and low speed signals shows the speed of myocardium at the place where they put Doppler pattern [10]. The pulse wave is used to determine the maximum speed of myocardium particularly along the longitudinal axis as the longitudinal fibers are parallel to the Doppler signal and the movement of the mitral annulus is a good surrogate for measuring the total longitudinal myocardial contraction and relaxation [10]. Visualization is obtained movement in systole and reverse two-phase movement long ossis toward apex in diastole and reverse biphase movement during isovolumic period [11].
Many studies are tested factors that affect LV systolic function at HTA patients. Sex is a strong correlate of body size and left ventricular mass (LVM) in HTA patients [12]. Studies have registered to cardiac size is influenced by body size, and for any given size, men have larger hearts than women, athletes have larger hearts than non-athletes, and obese subjects have larger hearts than non-obese subjects [13].
We are examined, in this study, known risk factors, according to studies which influenced the left ventricular hypertrophy, to identify risk factors the LV diastolic dysfunction (DD) in HTA that affect early heart damage independently from the HTA.
Methods
The echocardiographic testing was done on the machine Philips HD 11 probe 2.5 MHz. We used the parameters obtained by M-mode and 2-Dimensional (2D) echocardiography and Doppler echocardiography: End-Diastolic and End-Systolic dimension of the left ventricle (LV), wall thickness of LV were assessed M-mode, End-Diastolic (EDV), End-Systolic Volumes (ESV) were assessed 2-D echocardiography and LV ejection fraction (EF) according to Simpson' method.
Mitral flow was analysed by pulsed Doppler probe with 2.5 MHz we measured the maximum velocity of mitral flow, determined by the maximum speed of the mitral rapid filling (E wave) and the maximum rate of atrial contraction (A wave). Diastolic dysfunction was defined according to the American Society of Echocardiography the stages I of diastolic dysfunction were defined as E/A<0.8 [14].
Tissue Doppler quantifies regional myocardial function analysis of myocardial velocities at septal positions of the mitral annulus. Registered as S (maximum speed of positive waves registered in systole), Ea-wave maximum speed registered the rapid charging LV and maximum speed at atrial contraction (Aa). According's specifications echocardiographic Association of the European Society of Cardiology normal value for Sa and Ea waves is 8 cm/s (less than the average minus two standard deviations), the average value of 12 ± 2 cm/s, depending on age. Determined by the ratio of mitral E wave and Ea (E/Ea) for normal value was considered to be value <8. A normal BNP was 0-25.1 pmol/L.
Statistical Analysis
In the statistical analysis, we used descriptive statistic, and comparisons were performed for continuous variables by Student's t-test, chi-square test for categorical variables. For the calculation of the impacts of certain factors and echocardiographic parameters of the diastolic dysfunction was used one way Anova and Pearson´s or Spearman´s correlation. Parametric and nonparametric correlations were used to determine significant correlation between diastolic dysfunction and factors that could affect the diastolic dysfunction. Multivariate analysis was used to show the impact of risk factors on the LV diastolic dysfunction.
Results
The study included 419 patients with hypertension (HTA). Table 1 shows the baseline characteristics of patients, including therapy.
The average age of patients was 59.13 ± 10.141, male was present in 32%. Mean systolic blood pressure (BP) was 149.53 ± 21.846 and mean diastolic BP was 92.40 ± 11.399 (Stage 1), mean duration of HTA was 10.53 ± 8.53 years. Body mass index (BMI) showed that patients on average were overweight. The largest number of patients took ACE inhibitors (65.3%), and then beta blockers (BB) (53.6%), a combination of ACE inhibitors and diuretics have received 58.2% patients. Much less of patients were taking Ca blockers in 36.1% and angiotensin II receptors blockers (ARBs) in 5.5% of patients. Only 23% of HTA patients had dyspnoea. Mean BNP was in normal limits (Table 1).
| Characteristics | Number | Percentage (%) |
| Age | 59.13 ± 10.141 | |
| Male | 135 | 32.2 |
| BMI | 29.58 ± 4.94 | |
| Mean Systolic BP | 149.53 ± 21.846 | |
| Mean Diastolic BP | 92.40 ± 11.399 | |
| Mean Duration of HTA | 10.53 ± 8.53 years | |
| Beta blockers | 224 | 53.6 |
| ACE-inhibitors | 273 | 65.3 |
| ARBs | 23 | 5.5 |
| Ca blockers | 151 | 36.1 |
| Diuretics | 23 | 5.5 |
| ACE-inhibitors+diuretics | 242 | 58.2 |
| Dyspnea on effort | 47 | 11.2 |
| Dyspnea at rest | 52 | 12.4 |
| BNP | 11.6031 ± 11.20071 |
Table 1: Basal characteristics [BMI-Body Mass Index; BP-Blood Pressure; HTA-Hypertension; ACE-Angiotensin-Converting Enzyme; ARBs-Angiotensin II Receptors Blockers; ECC-Electrocardiogram; BNP-Braine Natriuretic Peptide]
Echocardiographic characteristics are on Table 2. All echocardiographic parameters were within normal limits. Number of HTA patients with EF<0.45 was 31 (7.4%), and number of HTA patients with diastolic dysfunction (DD) of 1 stage was 147 (35.1%). Number of HTA patients with >8 E/Ea<15 was 112 (26.7%) and with E/Ea>15 was 15 (3.6%) (Table 2).
| Characteristics | Mean | Std. Deviation |
| EDD | 48.231 | 27.338 |
| ESD | 31.739 | 11.3724 |
| Septum thickness | 9.99 | 5.432 |
| Posterior wall thickness | 10.126 | 7.6555 |
| EF | 58.66 | 9.434 |
| LA | 38.59 | 17.611 |
| E wave | 0.7609 | 0.20333 |
| A wave | 0.8505 | 0.2128 |
| E/A | 0.9326 | 0.33171 |
| Ea | 0.165 | 0.16773 |
| Aa | 0.1655 | 0.14411 |
| Sa | 0.1596 | 0.19788 |
| EF<0.45 | 31(7.4%) | |
| E/A<0.8 | 147 (35.1%) | |
| E/Ea | 6.3484 | |
| E/Ea>8-16 | 112 (26.7%) | |
| E/Ea>15 | 15 (3.6%) |
Table 2: Echocardiographic findings [EDD-End Diastolic Dimension; ESD-End Systolic Dimension; EF-Ejection Fraction; LA-Left Atrium Dimension; E wave-The Maximum Speed of the Mitral Rapid Filling; A wave-The maximum Rate of Mitral Late Filling; E/A ratio;Ea-Early Diastolic Mitral Annular Movement;Aa-Late Diastolic Mitral Annular Movement; Sa-Systolic Mitral Annular Movement; Index E/Ea-Relation the maximum speed of the Mitral Rapid Filling vs. the maximum speed of the Early Diastolic Mitral Annular Movement].
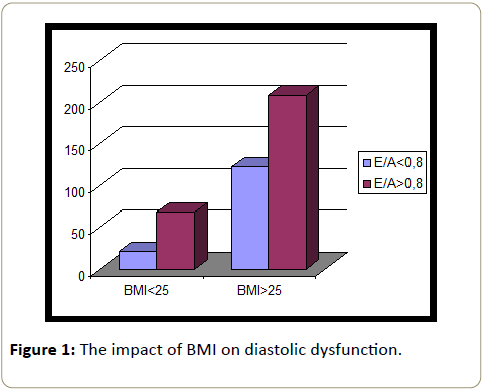
Figure 1 shows that the number of patients with diastolic dysfunction was significantly higher when they had a BMI >25 kg/m² than when they had a BMI <25 kg/m² (p<0.025).
Diabetes mellitus had no significant effect on the occurrence of LV diastolic dysfunction in hypertensive patients.
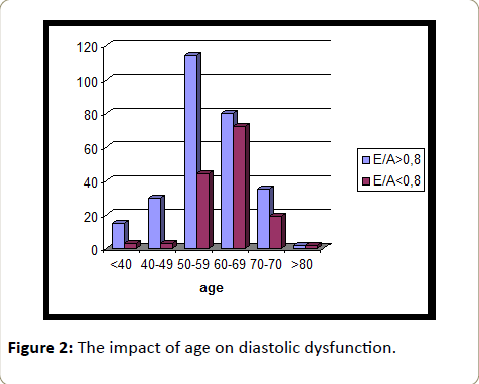
The hypertensive patients with diastolic dysfunction were significantly older (62.14 years vs. 52.57 years, p<0.001). Results showed that gender had no effect on LV diastolic dysfunction (Figure 1).
The difference is significant between the number of HTA patients with diastolic dysfunction age 40-49 years and age 50-59 years, between age 40-49 and HTA patients age 60-69 years ( p<0.001, p<0.033 respectively).
The differences also exist between the number of HTA patients with diastolic dysfunction age 50-59 years and age 60-69 years (p<0.005).
Most patients with hypertension aged 60-69 had a diastolic dysfunction (72/152-47.4%) (Figure 2).
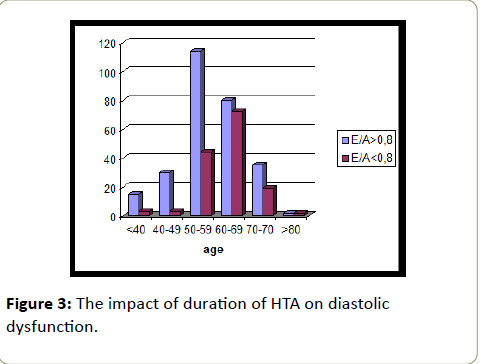
The differences exist between the number of HTA patients with diastolic dysfunction with 0-5 years of the duration of HTA and >10 years of duration of HTA (p<0.018). The HTA patients with a higher level of maximum systolic BP had significantly frequently diastolic dysfunction (190.66 vs. 183.27, p<0.005) (Figure 3).
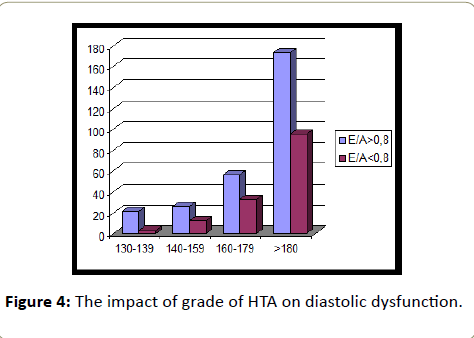
Grade of hypertension were not significantly affected diastolic dysfunction Correlation diastolic dysfunction and parameters of tissue Doppler (Ea wave) is significant at the p<0.01 level. Also significant correlation exists between diastolic dysfunction and Aa and Sa parameters of tissue Doppler (p<0.01, p<0.01 respectively).
Correlation diastolic dysfunction and age was found to significant level (p<0.01), then with higher level of maximum systolic BP (p<0.10) and with a ratio E/Ea (p<0.01). Nonparametric correlations it is found that there is also a significant correlation between diastolic dysfunction and left atrium dimension (p<0.05).
In a multivariate analysis, also of paramount influence on diastolic dysfunction were age (p=0.001) and higher level of maximum systolic BP (p=0.006) (Figure 4).
Discussion
According to data from the Cardiovascular Health Study (CHS) among participants of the study age ≥ 65 years is showed that subclinical cardiovascular disease (CVD) is very prevalent among older persons, substantially increases the risk of CVD among participants with hypertension or diabetes mellitus [15,16]. Therefore, we wanted to examine one of the functions of the heart- diastolic function of the heart in HTA patients.
HTA patients in our study were predominantly women (68%), mean BMI showed that they were overweight and the middle systolic/diastolic blood pressure was 149/92. These patients had average HTA 10 years, they had not well-regulated blood pressure (BP) and more than half were treated with combination therapy (ACE inhibitors+diuretics).
In addition to hypertrophy of the left ventricle (LV) which is one of the target organs that are damaged in HTA, HTA impairs diastolic function earlier and systolic function in the later stage of hypertensive heart disease [1]. Of our patients, only 7.4% had EF <0.45 and 35.1% diastolic dysfunction of 1 grade. The maximum speed of the mitral E wave determines trans mitral pressure gradient in early diastole When there is a prolonged LV relaxation and normal pressure in the LA, than there is a decrease in early mitral filling and E/A ratio <l [17]. Also, can be used tissue Doppler which measures of mitral annular velocity, systolic (S) and early (Ea) and late (Aa) velocity. The positive (above the zero line) systolic velocity of mitral annular motion registered by the apex and negative diastolic velocity that register movement along the longitudinal axis back to the lung veins Ea and Aa velocity representing LV filling [18]. In our study the average velocity of tissue Doppler parameters: Sa, Ea and Aa were in the normal range
However, therapy can influence the improvement of the Doppler parameters [19]. Antihypertensive therapy resulted in an increase in the prevalence of normal trans-mitral flow pattern from 28% to 46% of patients [19].
Our patients are in most cases treated with ACE inhibitors as monotherapy in 65.3% or as combination therapy with diuretics in 58.2% and perhaps this is one of the reasons that left ventricular hypertrophy was not represented to a greater extent and that diastolic dysfunction was present in only 1/3rd of patients.
In HTA patients, it was showed the value of E/Ea ratio, because that the 2013 ESC/ESH guidelines on arterial hypertension promote the use of E/Ea ratio in the detection of cardiac target organ damage in HTA [1,20,21]. In our study HTA patients had E/Ea ratio >8<15 in 26.7%, and >15 in 3.6%, but there was no correlation with symptoms of dyspnea and braine natriuretic peptide (BNP).
Diastolic Dysfunction
In addition to measuring the dimensions and volume and calculating EF, Doppler measurements are needed to determine hemodynamic state [22]. Mitral inflow measurements and tissue Doppler measurement in HTA patients can show delayed relaxation if there is diastolic dysfunction. Many studies are examined, also, the impact of factors such as obesity, age, gender and etc. on LV function in hypertensive patients.
Obesity
One study indicates a high prevalence of LVH in a cohort of obese women [13]. Based on the echocardiographic findings in the Framingham Heart Study it was concluded that there is an association between obesity and an increase in left ventricular mass [23].
Explanations for left ventricular hypertrophy in obesity are that obese individuals have an increase in intravascular volume and cardiac output, an increase in salt intake and a greater sympathetic activity also [24,25]. In our study the number of patients with diastolic dysfunction was higher when patients had a BMI>25 kg/m² than when they had a BMI<25 kg/m².
Results of the study, which examined the diastolic function in obese patients showed that the E/A was lower in obese subjects than in normal weight subjects and the risk of diastolic dysfunction was significantly higher in overweight subjects compared to normal weight subjects [26]. The Hypertension Genetic Epidemiology Network (HyperGEN) Study found the evidence of the strong association between increased fat-free mass and enhanced flow output, there is reason to suspect that the excess of fat mass might also contribute to the
Hemodynamic changes underlying both the development of arterial hypertension and the magnitude of LV mass at least in the context of obesity [26]. In moderate to severe cases of obesity, this may lead to left ventricular dilation, increased left ventricular wall stress [27]. The increase in cardiac output with obesity is caused by stroke volume, although because of increased sympathetic activation, heart rate is mildly increased as well [28].
In the study of Cesar et al, who investigated diastolic dysfunction in obese patients found that increased BMI was associated with worse LV diastolic function [29]. According to a cross-sectional population-based study of Millen et al assessing the impact of blood pressure and obesity on left-ventricular diastolic function, as assessed by conventional and tissue Doppler imaging (TDI) parameters it was concluded that if weight loss programmes fail to produce sustainable target body weights, rigorous BP management to lower than normal thresholds may be sufficient to prevent LV diastolic dysfunction [30].
Gender and age
Many studies indicate that men have greater LV volume and higher LVM than women [31]. Our results showed that gender had no effect on LV diastolic dysfunction.
The incidence of diastolic heart failure increases with age, 50% of older patients with heart failure may have isolated diastolic dysfunction [32]. Also, studies have registered to advanced years, in addition to sex, were significantly associated with a higher risk of LV remodelling [35]. The study examined risk factors for LV diastolic dysfunction that occurs over time in HTA, starting from the fact that the changes in LV function occur before symptoms is found that there was a significant decline in the E/A ratio with age and that the E/Ea ratio significantly increased with age [33].
There are explanations for the increase of LV wall thicknesses and LV cardiac diameters with advanced age, this is happening only in women because gender-specific hormones and the LV walls thickening without increasing the diameter LV could be the primary cause for LV mass increase in men with aging [34]. Our results showed that there is also a higher incidence of diastolic dysfunction in HTA patients with increasing age.
The duration and grade HTA
Studies that have examined the risk factors for LV diastolic dysfunction have found that the risk factor is systolic blood pressure (SBP) [35]. One study also found that the grade of diastolic dysfunction was significantly associated with increasing age and hypertension [36]. In our study there was a significant difference between diastolic dysfunction in hypertension patients who had hypertension >10 years duration in comparison to the HTA patients whose HTA last of the 5 years. The HTA patients with a higher level of maximum systolic BP had significantly frequently diastolic dysfunction.
However, grade of hypertension were not significantly affected diastolic dysfunction. In a multivariate analysis are also of paramount influence on diastolic dysfunction were age and higher level of maximum systolic BP. Traditional risk factors such as, obesity, age, hypertension has been associated with a higher frequency of diastolic dysfunction in HTA. Hence, it is essential aggressive modification of risk factors, particularly blood pressure control, weight loss to prevent or postponed LV diastolic dysfunction.
Conclusion
Left ventricular diastolic dysfunction in hypertensive patients could be prevented if the risk factors such as obesity and maximum height of systolic BP could be controlled so as to be within normal limits.
Acknowledgements
This study is sponsored by the Ministry of Health and Ministry of Science of Montenegro.
References
- Marwick HT, Gillebert CT, Aurigemma G, Chirinos J, Derumeaux G, et al. (2015) Recommendations on the use of echocardiography in adult hypertension: a report from the European Association of Cardiovascular Imaging (EACVI) and the American Society of Echocardiography (ASE).Eur Heart J Cardiovasc Imaging 28: 727-852.
- Gaasch WH, Zile MR (2011) Left ventricular structural remodelling in health and disease: with special emphasis on volume, mass, and geometry. J Am CollCardiol 58: 1733-1740.
- Beverly H,Lorell MD,Blase A (2000) Left ventricular hypertrophy pathogenesis, detection, and prognosis. Circulation102: 470-479.
- Weber KT, Brilla CG (1991) Pathologic hypertrophy and cardiac interstitium: fibrosis and renin-angiotensin-aldosterone system. Circulation83:1849-1865.
- Ho CY (2006) A clinician’s guide to tissue Doppler imaging. Circulation113:e396-e398.
- Ingels NB (1994) Left atrial pressure-clamp servomechanism demonstrates LV suction in canine hearts with normal mitral valves. Am J Physiol 267:H354-H362.
- Gradman AH, Wilson JT (2009) Hypertension and diastolic heart failure. CurrCardiol Rep11:422-429.
- Feigenbaum‘s Echocardiography. Philadelphia,USA (2005).
- Appleton CP (1993) Doppler assessment of left ventricular diastolic function:The refinements continue. J Am CollCardiol 21:1697-1700.
- Vinereanu D, Khokhar A, Fraser AG (1999) Reproducibility of pulsed wave tissue Doppler echocardiography. J Am SocEchocardiogr 12: 492-499.
- Gabriel W (2002) Tissue Doppler imaging in coronary artery disease. Heart views 3:3.
- Brumback LC, Kronmal R, Heckbert SR (2010) Body size adjustments for left ventricular mass by cardiovascular magnetic resonance and their impact on left ventricular hypertrophy classification. Int J Cardiovasc Imaging 26:459-468.
- Jennings G (2010) Obesity and left ventricular hypertrophy: does my heart look big on this? J Hypertens 28:2190-2193.
- Nagueh SF, Appleton CP, Gillebert TC, Marino PN, Oh JK, et al. (2009) Recommendations for the evaluation of left ventricular diastolic function byechocardiography. J Am SocEchocardiogr22: 107-133.
- Rosamond W, Flegal K, Furie K (2008) Heart disease and stroke statistics-2008 update: a report from the American heart association statistics committee and stroke statistics subcommittee. Circulation 117: e25-e146.
- Kleindorfer D, Broderick J, Khoury J (2006) The unchanging incidence and case-fatality of stroke in the 1990’s: a population-based study. Stroke 37: 2473-2478.
- Ishida Y (1986) Left ventricular filling dynamics influence of left ventricular relaxation and left atrial pressure.Circulation 74:187-196.
- Nagueh SF, Appleton CP, Gillebert TC, Marino PN, Oh JK (2009) Recommendations for the evaluation of left ventricular diastolic. Eur J Echocardiogr10:165-193.
- Wachtell K, Palmieri V, Gerdts E (2010) Prognostic significance of left ventricular diastolic dysfunction in patients with left ventricular hypertrophy and systemic hypertension. Am J Cardiol 106: 999-1005.
- Sharp AS, Tapp RJ, Thom SA (2010) Tissue Doppler E/E ratio is a powerful predictor of primary cardiac events in a hypertensive population: an ASCOT substudy. Eur Heart J 31:747-752.
- Mancia G, Fagard R, Narkiewicz K (2013) ESH/ESC guidelines for the management of arterial hypertension: the task force for the management of arterial hypertension of the European Society of Hypertension (ESH) and of the European Society of Cardiology (ESC). Eur Heart J 34:2159-2219.
- OmmenSR, NishimuraRA, AppletonCP (2000) Clinical utility of Doppler echocardiography and tissue Doppler imaging in the estimation of left ventricular filling pressures. A comparative simultaneous Doppler-catheterization study. Circulation 102: 1788-1794.
- Kannel WB, Gordon T, Offut D (1969) Left ventricular hypertrophy by electrocardiogram: prevalence, incidence and mortality in the Framingham study. Ann Intern Med 71: 89-105.
- Blake J, Devereux RB, Borer JS, Szule M, Pappas TW, et al. (1990) Relation of obesity, high sodium intake and eccentric left ventricular hypertrophy to left ventricular exercise dysfunction in essential hypertension. Am J Med 88: 477-485.
- Reisin E, Frohlich ED, Messerli FH (1983) Cardiovascular changes after weight reduction in obesity hypertension. Ann Intern Med 98: 315-319.
- Russo C, Jin Z, Homma S (2011) Effect of obesity and overweight on left ventricular diastolic function. J Am CollCardiol 57:1368-1374.
- PalmieriV, SimoneGD, ArnettDK (2001) Relation of various degrees of body mass index in patients with systemic hypertension to left ventricular mass, cardiac output, and peripheral resistance (The Hypertension Genetic Epidemiology Network Study). Am J Cardiol 88:1163-1168.
- AlpertMA (2001) Obesity cardiomyopathy: pathophysiology and evolution of the clinical syndrome. Am J Med Sci 321:225-236.
- MesserliFH, NunezBD, VenturaHO, SnyderDW (1987) Overweight and sudden death: increased ventricular ectopy in cardiomyopathy of obesity. Arch Intern Med 147: 1725-1728.
- Millen AME, Libhaber CD, Majane OHI, Libhaber E, Maseko MJ, et al. (2014) Relative impact of blood pressure as compared to an excess adiposity on left ventricular diastolic dysfunction in a community sample with a high prevalence of obesity. J Hypertens 32:2457-2464.
- Gardin JM, Wagenknecht LE, Culver HA, Flack J, Gidding S, et al. (1995) Relationship of cardiovascular risk factors to echocardiographic left ventricular mass in healthy young black and white adult men and women. The CARDIA study. Circulation 92:380-387.
- Satpathy C, Mishra TK, Satpathy R (2006) Diagnosisand management of diastolic dysfunction and heart failure. Am Fam Physician73:841-846.
- Gjesdal O, Bluemke DA, Lima JA (2011) Cardiac remodeling at the population level--risk factors, screening, and outcomes. Nat Rev Cardiol 8:673-685.
- Kuznetsova T, Herbots L, Lopez B (2009) Prevalence of left ventricular diastolic dysfunction in a general population. Circulation: Heart Failure 2:105-112.
- Chen C, Sung KT, Shih SC (2016) Age, gender and load-related influences on left ventricular geometric remodeling, systolic mid-wall function, and nt-probnp in asymptomatic asian population. PLoS One 11: e0156467.
- AlJaroudi W, Alraies MC, Halley C (2012) Impact of progression of diastolic dysfunction on mortality in patients with normal ejection fraction. Circulation125:782-788.
Open Access Journals
- Aquaculture & Veterinary Science
- Chemistry & Chemical Sciences
- Clinical Sciences
- Engineering
- General Science
- Genetics & Molecular Biology
- Health Care & Nursing
- Immunology & Microbiology
- Materials Science
- Mathematics & Physics
- Medical Sciences
- Neurology & Psychiatry
- Oncology & Cancer Science
- Pharmaceutical Sciences