Skin Ultrasonography and Color Doppler as a Diagnostic Technique for Non-Melanocytic Skin Tumors
Maria Elena Del Prado Sanz1*, Ricardo Ruiz-Villaverde2, Priscilla Giavedoni3, Ana Rodriguez4, David Vidal5, Fernando Alfajeme6 and Daniel Bordonaba7
1Department of Dermatology, Hospital General San Jorge, Huesca, Spain
2Department of Dermatology, Virgin of the Snows Hospital, Granada, Spain
3Department of Dermatology, Clinical Hospital of Barcelona, Barcelona, Spain
4Department of Dermatology, Hospital La Paz, Madrid, Spain
5Department of Dermatology, Sant Joan Despi Moises Broggi Hospital, Barcelona, Spain
6Department of Dermatology, Puerta de Hierro Majadahonda University Hospital, Majadahonda, Spain
7Department of Dermatology, Aragon Institute of Health Sciences, Zaragoza, Spain
- *Corresponding Author:
- Maria Elena Del Prado Sanz
Department of Dermatology,
Hospital General San Jorge,
Huesca,
Spain;
Email: melenadelprado@gmail.com
Received: July 14, 2020, Manuscript No. IPIBP-23-5191; Editor assigned: July 17, 2020, PreQC No. IPIBP-23-5191 (PQ); Reviewed: July 31, 2020, QC No. IPIBP-23-5191; Revised: September 15, 2023, Manuscript No. IPIBP-23-5191 (R); Published: October 13, 2023, DOI: 10.36648/2471-9897.9.2.51
Citation: Del Prado Sanz ME, Ruiz-Villaverde R, Giavedoni P, Rodriguez A, Vidal D, et al. (2023) Skin Ultrasonography and Color Doppler as a Diagnostic Technique for Non-Melanocytic Skin Tumors. Insights Blood Press Vol.9 No.2: 51.
Abstract
Introduction: The introduction of new diagnostic imaging techniques in dermatology, such as cutaneous B-mode ultrasonography (ultrasound/ecography) with color doppler, could improve the diagnosis of non-melanocytic tumors, mainly of those that are intradermal and subcutaneous lesions. The overall objective of this study was to evaluate the validity and diagnostic accuracy of dermatologic highfrequency ultrasound as a test for diagnosing bening, melanocytic skin neoplasms. A more specific objective was to gauge the sensitivity and specificity of dermatologic ultrasound as measures of its own validity, by using the diagnostic-therapeutic biopsy as a gold standard test.
Materials and methods: This is a multicenter prospective cohort study, which involved 642 patients from 4 different Spanish cities, along with 6 participating hospitals, 6 medical-surgical dermatologists and dermatological ultrasound experts and 6 anatomical-pathologists (pathologists) that are also experts in dermatologic histopathology.
Results: The main objective of the estimated variables’ study was achieved, with a 95% Confidence Interval (CI). Ultrasound’s sensitivity to detect benign non-melanocytic skin lesions-0.93 (0.89, 0.14); ultrasound’s specificity to detect malignant non-melanocytic skin tumors-0.84 (0.79, 0.88); Positive Predictive Value (PPV)-0.84 (0.80, 0.88); Negative Predictive Value (NPV)-0.92 (0.88, 0.95); Positive Likelihood Ratio (PLR) or correct hit-ratio (correctly classified tumors)-5.66 (4.33, 7.38); Negative Likelihood Ratio (NLR) or incorrect hit-ratio (misclassified tumors)-0.09 (0.06, 0.14).
Conclusion: Dermatologic high-resolution ultrasound is a valid and safe enough test that can be used when diagnosing non-melanocytic skin tumors.
Keywords
Ultrasonography; Diagnostic imaging; Skin neoplasms; Dermatology; Biopsy; Pathology
Introduction
Research in context
Existing evidence before this study: In order to examine the issue of surgical over-intervention in patients with benign nonmelanocytic tumors, we performed a previous retrospective study in which we analyzed surgical anatomic-pathology reports of lesion samples, whose initial diagnosis suggested that surgery was recommended. After 131 analyzed samples over a 12- month period, the definitive diagnosis by "Gold standard" test of anatomic pathology yielded the following data: 76 (58%) were benign (therefore initial ones that wouldn’t have required surgery), 55 (42%) were malignant (correct surgical treatment) [1].
From these data it follows that 58% of the patients were unnecessarily treated with surgery. These data made it necessary to analyze the possibilities of dermatologic highresolution ultrasound in order to avoid needless surgery, inconvenience for patients and the consumption of unneeded resources from the health system for not having a diagnostic technique that complements those that have been used so far. Many of the extirpated injuries pose no risk of malignant transformation and a simple tracking or a biannual ultrasound control that could track their size would be enough, thereby avoiding risks of surgical wound infections, cures and other care from nursing services and/or primary care. This would also contribute to a decrease in the amount of minor and local surgeries, resulting in a reduction of the surgical waiting list and savings for public health, since each local surgery is estimated at approximately € 150 per intervention [2].
We conducted a literature search in PubMed using the terms: “Dermatological ultrasound” and “skin tumors” and found that the presence of increasingly well-characterized ultrasound patterns can guide us greatly to complement clinical diagnosis in cases where the technique is applicable and can help reduce unnecessary surgeries. Ultrasound patterns within the tumor pathology section have been described as follows:
Epidermal cyst: Hypoechoic oval mass, with a duct called punctum-that connects to the surface and posterior acoustic reinforcement.
Pilomatrixoma: Hyperechoic solid mass with a hypoechoic halo and punctate calcifications, with rear acoustic shadowing [3]. It may present some degree of vascularization around.
Lipomas: They are typical when their content is exclusively fat and appear as markedly hyperechoic oval masses following the transverse axis of the skin layers. Lipomas are atypical when they are also associated with connective (fibrolipomas) or capillary (angiolipoma) tissue [4].
Additional value provided by this study
To our knowledge, this is the first multicenter national and international study that demonstrates with scientific rigor the sensitivity, specificity, internal and external validity of dermatologic doppler ultrasound in the diagnosis of nonmelanocytic skin tumors [5].
Consequences of all of the available evidence
Dermatologic high-resolution ultrasound is valid and safe enough diagnostic test to be used in the clinical practice of diagnosing a non-melanocytic skin tumor lesion. When used in the previous diagnosis of a non-melanocytic skin tumor lesion, dermatologic high-resolution ultrasound may allow avoiding the performance of unnecessary surgery in patients that are usually operated by following a clinical impression [6].
Ultrasound is based on the physical principles of highfrequency sound: Inaudible sounds whose frequencies are above 20,000 Hz. They are produced by ultrasonic transducer crystals that have the ability to make such waves in response to the electric current and convert the reflected echo from these ultrasounds into electrical signals, through the effect known as piezoelectric effect. Dermatology is interested in very superficial structures and the discrimination with imaging resolution of their components’ echoes. Therefore, suitable equipment consists of high-frequency probes (above 15 MHz). Scanning probes must be linear, since we are interested in structures that are parallel to the body surface. Through the doppler effect (the frequency change of the emitted sound when it gets reflected on the moving erythrocytes), we are able to detect the skin structures’ blood flow that has been incremented due to cutaneous inflammation and neovascularization [7].
From a clinical point of view, there are basically two different groups of benign cutaneous tumors: Melanocytic and nonmelanocytic lesions-a division that will influence their diagnosis and therapeutic management. For the approach of the first type, there is a morphological description technique that is already developed and widely introduced in our daily clinical practice: Dermoscopy or dermatoscopy. Over the last 20 years, multiple dermatoscopic and morphological criteria has been described, which allows for an early diagnosis of malignant melanoma, just like patterns that can be used to distinguish the different types of nevi, thereby enabling the decrease of misdiagnosis in the presence of clinically unclear lesions depending, of course, on the examiner’s experience and knowledge on patterns and algorithms. However, dermoscopy, which allows for the evaluation of these lesions, either has no indication in benign subcutaneous tumoral lesions since they are covered by normal skin or is limited if there are diagnostic doubts because the tumor does not show characteristic dermoscopic findings [8].
The introduction of new diagnostic techniques, such as cutaneous B-mode ultrasound and color dopple have improved both the sensitivity and specificity of the diagnosis of thesemainly subcutaneous-benign tumor lesions, by increasing its precision by almost 20%. It is a technique that helps us define their best characterization (location and size), their relationship to adjacent structures, their degree of vascularization, an adequate surgical planning only in those cases where it is necessary and the avoidance of surgery in many of the lesions. It is a safe technique for the patient and it provides a careful differential diagnosis in clinically unclear cases, allowing for minor outpatient surgery techniques, such as ultrasound-guided biopsies, drains, infiltrations and removals of foreign bodies [9,10].
Materials and Methods
Design and participants in the study
This is a prospective validation study in which a cohort of subjects without definite diagnosis undergo the test under validation (ultrasound and dermatologic doppler) at first, to then continue until reaching a definitive diagnosis through surgery, plus Anatomic Pathology (AP), according to standard practice [11].
The study was conducted in non-melanocytic nodular tumor lesions, classified into two groups: Benign and malignant. Patients were selected from dermatology services with skin ultrasound and color doppler units: Huesca’s San Jorge hospital, Madrid’s Puerta de Hierro Majadahonda hospital Madrid, Madrid’s la Paz hospital, Barcelona’s clinic hospital, Barcelona’s Sant Joan Despi Moises Broggi hospital and Granada’s Virgen de las Nieves hospital [12].
Adult patients ≥ 18 years old), with non-melanocytic nodular skin tumors-sized from 0.5 mm to 10 cm, were considered to be participants of this study. All researchers used esaote my lab ultrasoundequipment, with 18 MHz straight probes that had a 0.2 resolution. A complete list of inclusion and exclusion criteria is included in appendix [13].
The studies were conducted according to the Good Clinical Practice (GCP) standards that regulate the conduct of clinical studies and the ethical principles set out in the declaration of Helsinki. All documents related to the study (including the study’s protocols) were approved by an internal review council or ethics committee of independent investigation from each of the centers and all patients gave written informed consent prior to their participation in the study [14].
Randomization and masking
The prospective nature of this study and the fact of applying the test before making the inal diagnosis also allows for control of the main biases, thereby ensuring: The independent evaluation of the test under validation and the diagnostic test to which it is compared; and also that all participants, regardless of their results, are subject to the full diagnostic process. In addition, this will enable us to measure both the sensitivity and speci icity as positive and negative predictive values and other valuation parameters, since all marginal values from the ieldwork table are random and therefore it assures us to also be able to calculate the prevalence of the entity being measured. Researchers from the anatomic pathology departments, who received the samples under analysis, remained blinded during the study [15].
Procedures
During the irst year of study (2017), we recruited patients and collected their signed informed consent forms. Subsequently, we performed the test under study skin ultrasound plus Data Collection Logbook (DCL) illing.
Lastly, when surgeries were scheduled, we proceeded to the surgical removals and the shipment of samples to the anatomic pathology department. During the second year (2018), we conducted the study and anatomical-pathological diagnosis of surgical specimens with DCL illing and, later on, the collection of data from all of the researchers.
During the third and inal year (2019), we completed the statistical analysis, the development of the test and the analysis of the results.
Valuation parameters
The main b-mode and color doppler ultrasound evaluation variables were: 1) Lesion size (<5 mm: High suspicion of benignity and ≥ 5 mm: High suspicion of malignancy; 2) echogenicity of the tissue proximate to the tumor (normal high suspicion of benignity and altered: High suspicion of malignancy); 3) vascularization of the lesion (absent high suspicion of benignity and present high suspicion of malignancy).
Secondary ultrasound evaluation variables-in order of assessment were as follows: 1) Echogenicity of the lesion (homogeneous: High suspicion of benignity and heterogeneous: High suspicion of malignancy); 2) borders (well-defined: High suspicion of benignity, ill-defined: High suspicion of malignancy); 3) morphology (rounded: High suspicion of benignity, multilobed: High suspicion of malignancy).
Statistical analysis
All three ultrasound test, surgical removal and subsequent pathological study, were conducted in the 642 patients included in the study, distributed in 6 hospitals within the Spanish national territory (Table 1).
| Name/Center | (ALL) N=642 |
|---|---|
| Clinic universitary hospital | 162 (25.27%) |
| Sant Joan Despi Moises Broggi hospital | 20 (3.12%) |
| San Jorge general hospital | 105 (16.38%) |
| La Paz university hospital | 59 (9.20%) |
| Puerta de Hierro Majadahonda university hospital | 144 (22.46%) |
| Vírgen de las Nieves university hospital | 151 (23.56%) |
| Date of birth | 01-Jun-1955 (13-Jun-1944; 27-Aug-1970) |
| Dates of ultrasound tests | 25-Jul-2018 (01-Feb-2018; 16-Jan-2019) |
| Age | 63.00 (48.00, 74.00) |
| Gender | |
| Woman | 318 (49.61%) |
| Man | 323 (50.39%) |
| Borders | |
| Well-defined | 461 (71.92%) |
| Ill-defined | 180 (28.8%) |
| Shape shape | |
| Oval | 348 (54.29%) |
| Rounded | 293 (45.71%) |
| Shape border | |
| Irregular | 247 (38.53%) |
| Regular | 394 (61.47%) |
| Shape morphology | |
| Lobed | 589 (91.89%) |
| Multi-lobed | 52 (8.11%) |
| Location | |
| Superficial | 369 (57.57%) |
| Deep | 272 (42.43%) |
| Size | 8.00 (6.00, 13.00) |
| Size 2 | |
| Benign <5 mm | 70 (10.92%) |
| Malignant ≥ 5 mm | 571 (89.08%) |
| US (ultrasound) lesion hypo | |
| No | 73 (11.39%) |
| Yes | 568 (88.61%) |
| US lesion hyper | |
| No | 464 (72.39%) |
| Yes | 177 (27.61%) |
| US lesion iso | |
| Yes | 64 (9.98%) |
| No | 577 (90.02%) |
| US lesion | |
| Homogeneous | 483 (75.35%) |
| Heterogeneous | 158 (24.65%) |
| US post reinforcement | |
| No | 511 (79.72%) |
| Yes | 130 (20.28%) |
| US post acoustic shadow | |
| No | 565 (88.14%) |
| Yes | 76 (11.86%) |
| US tissue | |
| Normal | 486 (75.82%) |
| Altered | 155 (24.18%) |
| Vascularization | |
| Absent | 257 (40.09%) |
| Multifocal intralesional | 152 (23.71%) |
| Multifocal peripheral | 112 (17.47%) |
| Unifocal peripheral | 120 (18.72%) |
| Vascularizacion group | |
| Benign | 377 (58.81%) |
| Malignant | 264 (41.19%) |
| Calcifications | |
| Absent | 592 (92.36%) |
| Present | 49 (7.64%) |
| Dermatologic judgement | |
| High suspicion of benignity | 345 (53.82%) |
| High suspicion of malignancy | 296 (46.18%) |
| AP date of intervention | 01-Oct-2018 (15-Feb-2018; 07-Feb-2019) |
| AP date of report | 08-Oct-2018 (07-Mar-2018; 21-Feb-2019) |
| AP growth | |
| Expansive | 427 (66.61%) |
| Infiltrating | 214 (33.39%) |
| AP necrosi | |
| Absent | 557 (86.90%) |
| Present and abundant | 15 (2.34%) |
| Present and poor | 69 (10.76%) |
| AP ulceration | |
| Absent | 531 (82.84%) |
| Present and abundant | 40 (6.24%) |
| Present and poor | 70 (10.92%) |
| AP nucleus cytoplasm | |
| Increased | 0280 (43.68%) |
| Non-increased | 361 (56.32%) |
| AP mitosis | |
| Scarce atypical | 144 (22.46%) |
| Scarce typical | 384 (59.91%) |
| Common atypical | 58 (9.05%) |
| Common typical | 55 (8.58%) |
| AP vacularization distribution | |
| Irregular | 278 (43.37%) |
| Regular | 363 (56.63%) |
| AP anatomical pathology judgement | |
| High suspicion of benignity | 371 (57.88%) |
| High suspicion of malignancy | 270 (42.12%) |
| Vascularization 2 | |
| Benign | 377 (58.81%) |
| Malignant | 264 (41.19%) |
Table 1: Summary descriptives.
In order to evaluate the effect of protocol deviations in the analysis of the main variables, the following methodology was used for statistical analysis of the data:
Univariate descriptive statistics: The qualitative variables are displayed by the frequency distribution of each category’s percentages. As for the quantitative variables-age and size, it was observed that they do not follow a normal distribution by using the Shapiro-Wilks test and median and first and third quartiles were set as descriptive measures.
Inferential statistics: The association between anatomical pathology’s factors and diagnosis-considered a gold standard test was analyzed by using hypothesis testing, with comparison of proportions when the factors were qualitative variables (chisquare, Fisher ‘s exact test) and with a nonparametric test (Mann-Whitney U test) when the factors were quantitative variables.
Analysis was completed with univariate and multivariate logistic regression models. OR measurement, 95% Confidence Interval (CI) and p-value of each variable are indicated. Specific techniques were used for the study of diagnostic tests these are validity indicators, such as sensitivity, specificity, predictive values and likelihood ratios. Sofware R (a) and compareGroups libraries (b) were used.
Results
Ultrasound tests were run on the total 642 patients between February 1, 2018 and January 1, 2019. Surgical excisions of the 642 nodular tumors under study were performed between February 15, 2018 and February 7, 2019. An Anatomical- Pathological study (AP) of the 642 samples that were blindly remitted the anatomical-pathologists was conducted to from March 7, 2018 until February 21, 2019. Therefore, a total of 642 patients were included in the study and they completed it.
Demographic parameters and characteristics of the population under study at baseline situation were generally well-balanced, where the mean age of participants was 63 years. The descriptive statistics performed on the primary and secondary variables is described with the mean and the Standard Deviation-mean (SD)-in continuous variables, while qualitative or categorical variables are presented as frequencies and percentages in each category (Table 2).
| Variables | High suspicion of benignity | High suspicion of malignancy | OR (Univariate) | OR (multivariable) | ||
|---|---|---|---|---|---|---|
| Model 1 | Age | Mean (SD) | 51.9 (16.9) | 71.8 (11.9) | 1.09 (1.08-1.11, p<0.001) | 1.08 (1.07-1.10, p<0.001) |
| Gender | Woman | 205 (55.3) | 113 (41.9) | - | - | |
| Man | 166 (44.7) | 157 (58.1) | 1.72 (1.25-2.36, p=0.001) | 1.73 (1.15-2.61, p=0.008) | ||
| Size 2 | Benign <5 mm | 50 (13.5) | 20 (7.4) | - | - | |
| Malignant ≥ 5 mm | 321 (86.5) | 250 (92.6) | 1.95 (1.15-3.42, p=0.016) | 2.15 (1.11-4.28, p=0.026) | ||
| US_lesion | Homogeneous | 307 (82.7) | 176 (65.2) | - | - | |
| Heterogeneous | 64 (17.3) | 94 (34.8) | 2.56 (1.78-3.71, p<0.001) | 1.13 (0.66-1.91, p=0.651) | ||
| US_tissue | Normal | 329 (88.7) | 157 (58.1) | - | - | |
| Altered | 42 (11.3) | 113 (41.9) | 5.64 (3.80-8.50, p<0.001) | 2.25 (1.36-3.75, p=0.002) | ||
| US_lesion_iso | Yes | 50 (13.5) | 14 (5.2) | - | - | |
| No | 321 (86.5) | 256 (94.8) | 2.85 (1.58-5.46, p=0.001) | 1.77 (0.78-4.25, p=0.188) | ||
| Vascularization_group | Benign | 272 (73.3) | 105 (38.9) | - | - | |
| Malignant | 99 (26.7) | 165 (61.1) | 4.32 (3.09-6.06, p<0.001) | 2.41 (1.54-3.77, p<0.001) | ||
| Model 2 | Age | Mean (SD) | 51.9 (16.9) | 71.8 (11.9) | 1.09 (1.08-1.11, p<0.001) | 1.09 (1.07-1.10, p<0.001) |
| Gender | Woman | 205 (55.3) | 113 (41.9) | - | - | |
| Man | 166 (44.7) | 157 (58.1) | 1.72 (1.25-2.36, p=0.001) | 1.73 (1.15-2.60, p=0.008) | ||
| Size 2 | Benign <5 mm | 50 (13.5) | 20 (7.4) | - | - | |
| Malignant ≥ 5 mm | 321 (86.5) | 250 (92.6) | 1.95 (1.15-3.42, p=0.016) | 2.09 (1.08-4.17, p=0.031) | ||
| US_tissue | Normal | 329 (88.7) | 157 (58.1) | - | - | |
| Altered | 42 (11.3) | 113 (41.9) | 5.64 (3.80-8.50, p<0.001) | 2.25 (1.36-3.77, p=0.002) | ||
| US_lesion | Homogeneous | 307 (82.7) | 176 (65.2) | - | - | |
| Heterogeneous | 64 (17.3) | 94 (34.8) | 2.56 (1.78-3.71, p<0.001) | 1.07 (0.63-1.81, p=0.787) | ||
| Vascularization_group | Benign | 272 (73.3) | 105 (38.9) | - | - | |
| Malignant | 99 (26.7) | 165 (61.1) | 4.32 (3.09-6.06, p<0.001) | 2.44 (1.56-3.82, p <0.001) | ||
| Model 3 | Age | Mean (SD) | 51.9 (16.9) | 71.8 (11.9) | 1.09 (1.08-1.11, p<0.001) | 1.09 (1.07-1.10, p<0.001) |
| Gender | Woman | 205 (55.3) | 113 (41.9) | - | - | |
| Man | 166 (44.7) | 157 (58.1) | 1.72 (1.25-2.36, p=0.001) | 1.72 (1.15-2.59, p=0.008) | ||
| Size 2 | Benign <5 mm | 50 (13.5) | 20 (7.4) | - | - | |
| Malignant ≥ 5 mm | 321 (86.5) | 250 (92.6) | 1.95 (1.15-3.42, p=0.016) | 2.09 (1.08-4.16, p=0.031) | ||
| US_tissue | Normal | 329 (88.7) | 157 (58.1) | - | - | |
| Altered | 42 (11.3) | 113 (41.9) | 5.64 (3.80-8.50, p<0.001) | 2.29 (1.41-3.77, p=0.001) | ||
| Vascularization_group | Benign | 272 (73.3) | 105 (38.9) | - | - | |
| Malignant | 99 (26.7) | 165 (61.1) | 4.32 (3.09-6.06, p<0.001) | 2.49 (1.63-3.80, p<0.001) | ||
| Model 3 | Age | Mean (SD) | 51.9 (16.9) | 71.8 (11.9) | 1.09 (1.08-1.11, p<0.001) | 1.09 (1.07-1.10, p<0.001) |
| Gender | Woman | 205 (55.3) | 113 (41.9) | - | - | |
| Man | 166 (44.7) | 157 (58.1) | 1.72 (1.25-2.36, p=0.001) | 1.72 (1.15-2.59, p=0.008) | ||
| Size 2 | Benign <5 mm | 50 (13.5) | 20 (7.4) | - | - | |
| Malignant ≥ 5 mm | 321 (86.5) | 250 (92.6) | 1.95 (1.15-3.42, p=0.016) | 2.09 (1.08-4.16, p=0.031) | ||
| US_tissue | Normal | 329 (88.7) | 157 (58.1) | - | - | |
| Altered | 42 (11.3) | 113 (41.9) | 5.64 (3.80-8.50, p<0.001) | 2.29 (1.41-3.77, p=0.001) | ||
| Vascularization_group | Benign | 272 (73.3) | 105 (38.9) | - | - | |
| Malignant | 99 (26.7) | 165 (61.1) | 4.32 (3.09-6.06, p<0.001) | 2.49 (1.63-3.80, p<0.001) | ||
Table 2: AP Anatomical Pathology judgement.
Comparing the groups with anatomical pathology’s judgment showed significant differences in primary variables under study: Lesion size, echogenicity of surrounding tissue and vasculature of the lesion; also significant differences in the secondary variables-age, gender, echogenicity of the lesion were found.
Patients with a mean age of 52 years had a higher number of lesions with high suspicion of benignity, whereas patients with a mean age of 72.5 years had a greater number of lesions with high suspicion of malignancy, i.e., the age of 72 years or older is a risk factor for lesions with suspicion of malignancy.
A lesion size greater than 5 mm is a risk factor for high suspicion of malignancy, having a 94% greater risk of high suspicion for malignancy. The location of the lesions (deep: reticular dermis and subcutaneous tissue) was not a significant variable (p-value=0222 and OR=0.82), although it indicates that deep lesions have an 82% greater risk of high-malignancy suspicion than superficial ones. This previous data, applied to the usual clinical practice could be explained, as it corresponds to existent lesions with criteria of malignancy and also infiltrative, invasive and rapid growth, where the depth would be a risk factor for malignancy. However, there exist nodular tumors of benign cystic nature (located in reticular dermis) and hypodermis lesions (lipomas) also benign but located more deeply in subcutaneous and reticular dermis, which could explain their not significant p-value. As for the echogenicity inside the lesion itself (secondary variable classified in: Hypoechoic, hyperechoic or isoechoic), the results prove that isoechogenicity loss has 2.8-fold more risk of high suspicion for malignancy than isoechogenic lesions do. Examples of benign nodular tumors that match this result are: Dermatofibromas and lipomas-which have a similar echogenicity to the tissue in which they settle or are surrounded by.
Another primary variable of the study is the echogenicity of surrounding tissue and the results show that lesions with an altered echogenicity of the tissue has a 5.6 times higher risk for high suspicion of malignancy than lesions that had a normal echogenicity of surrounding tissue. The presence of vascularization in lesions with a 4.30 OR is one of the primary variables under study that proves that vascularized lesions have a 4.3 times greater risk of high suspicion for malignancy than non-vascularized ones (Table 3).
| Variables | ALL (N=641) | High suspicion of benignity (N=371) | High suspicion of malignancy (N=270) | OR | p-value |
|---|---|---|---|---|---|
| Age | 63.0 (48.0; 74.0) | 52.0 (40.0; 65.0) | 72.5 (65.0; 81.0) | 1.09 (1.08; 1.11) | <0.001 |
| Gender | |||||
| Woman | 318 (49.6%) | 205 (55.3%) | 113 (41.9%) | Ref. | Ref. |
| Man | 323 (50.4%) | 166 (44.7%) | 157 (58.1%) | 1.71 (1.25; 2.36) | 0.001 |
| Location | |||||
| Superficial | 369 (57.6%) | 206 (55.5%) | 163 (60.4%) | Ref. | Ref. |
| Deep | 272 (42.4%) | 165 (44.5%) | 107 (39.6%) | 0.82 (0.60; 1.13) | 0.222 |
| Size | 8.00 (6.00; 13.0) | 8.00 (6.00; 5.13) | 8.00 (6.00; 12.0) | 0.99 (0.98; 1.00) | 0.067 |
| Size 2 | |||||
| Benign <5 mm | 70 (10.9%) | 50 (13.5%) | 20 (7.41%) | Ref. | Ref. |
| Malignant ≥5 mm | 571 (89.1%) | 321 (86.5%) | 250 (92.6%) | 1.94 (1.14; 3.41) | 0.014 |
| US_lesion | |||||
| Homogeneous | 483 (75.4%) | 307 (82.7%) | 176 (65.2%) | Ref. | Ref. |
| Heterogeneous | 158 (24.6%) | 64 (17.3%) | 94 (34.8%) | 2.56 (1.77; 3.71) | <0.001 |
| US_lesion_hypo | |||||
| No | 73 (11.4%) | 67 (18.1%) | 6 (2.22%) | Ref. | Ref. |
| Yes | 568 (88.6%) | 304 (81.9%) | 264 (97.8%) | 9.45 (4.36; 25.0) | <0.001 |
| US_lesion_hyper | |||||
| No | 464 (72.4%) | 285 (76.8%) | 179 (66.3%) | Ref. | Ref. |
| Yes | 177 (27.6%) | 86 (23.2%) | 91 (33.7%) | 1.68 (1.19; 2.39) | 0.003 |
| US_lesion_iso | |||||
| Yes | 64 (9.98%) | 50 (13.5%) | 14 (5.19%) | Ref. | Ref. |
| No | 577 (90.0%) | 321 (86.5%) | 256 (94.8%) | 2.82 (1.56; 5.43) | <0.001 |
| US_tissue | |||||
| Normal | 486 (75.8%) | 329 (88.7%) | 157 (58.1%) | Ref. | Ref. |
| Altered | 155 (24.2%) | 42 (11.3%) | 113 (41.9%) | 5.61 (3.78; 8.47) | 0.000 |
| Vascularization_group | |||||
| Benign | 377 (58.8%) | 272 (73.3%) | 105 (38.9%) | Ref. | Ref. |
| Malignant | 264 (41.2%) | 99 (26.7%) | 165 (61.1%) | 4.30 (3.08; 6.04) | 0.000 |
| Dermatology_judgement | |||||
| High suspicion of benignity | 345 (53.8%) | 325 (87.6%) | 20 (7.41%) | Ref. | Ref. |
| High suspicion of malignancy | 296 (46.2%) | 46 (12.4%) | 250 (92.6%) | 86.6 (51.0, 154) | 0.000 |
Table 3: Summary descriptives table by groups of ‘AP anatomical pathology judgement’.
Three multivariate regression models were used, with the following results:
Model 1: Nodular skin tumors in men have a 73% greater risk of high suspicion for malignancy than they do in women. As for the main size variable, the multivariate analysis indicates that the risk of showing high suspicion for malignity is increased 2.1- fold in lesions that are larger than 5 mm. One of the secondary variables analyzed in this model 1 was the echogenicity of the lesion, globally classified as homogeneous (similar echogenicity in the lesion’s composition, with one of the possible components-liquid, solid, calcic, etc. being predominant) and heterogeneous (different echogenicities within the same lesionliquid, solid and calcic). The results in this case showed that lesions with heterogeneous echogenicity continued to have a 13% greater risk of high suspicion for malignancy, a result that differs from the previous univariate analysis, where lesions with heterogeneous echogenicity had a 2.5 times higher risk of high suspicion for malignancy. Therefore, this secondary variable is not useful by itself to help us discern between the suspicion of benignity or malignancy, since benign lesions-such as sebaceous and/or epidermal cysts-have different echogenicities (hypoechoic and hyperechoic) and similarly, malignant lesionssuch as squamous cell carcinoma and basal cell carcinoma-have heterogeneous echogenicity. Once again, multivariate model 1’s primary variable-the echogenicity of the tissue surrounding the lesion, still has up to 2.2-times increased risk of high suspicion for malignancy when altered. Similarly, the vascularization in the nodular-tumoral lesions that are being studied maintains its pvalue< 0.001, with a multivariable OR of 2.4 (1.54-3.77).
Model 2 and model 3: The research study’s primary variables size of the lesion, echogenicity of surrounding or perilesional tissue and vascularization of the lesion, along with two secondary variables-age and sex, are analyzed. Results show a statistically significant value for these three described variables. One of the other conducted analyses even though it was not the goal of this study and therefore, its interpretation should be cautious, was that of the relationships between anatomical pathology and dermatology’s variables (Table 4). Thus, we found significant connections between anatomical pathology’s primary variable of a tumor’s infiltrative growth and other primary variables from the test under study, such as the echogenicity of the surrounding tissue with a 2.80 (1.93; 4.07) OR and a <0.001 p-value and the vascularization shown in the ultrasound images with a 1. 82 (1.30; 2.45) OR and a <0.01 p-value. The present research study has reached its primary goal on the estimated variables, with a 95% CI. Cutaneous ultrasound and doppler’s sensitivity to detect non-melanocytic benign skin lesions-0.93 (0.89, 0.14); ultrasound’s specificity to detect non-melanocytic malignant skin tumors-0.84 (0.79, 0.88); Positive Predictive Value (PPV)-0.84 (0.80, 0.88); Negative Predictive Value (NPV)-0.92 (0.88, 0.95); Positive Likelihood Ratio (PLR) or correct hit-ratio (correctly classified tumors): 5.66 (4.33, 7.38); Negative Likelihood Ratio (NLR) or incorrect hit-ratio (misclassified tumors): 0.09 (0.06, 0.14).
Discussion
The results of this prospective validation study in a cohort of subjects without a definitive diagnosis, indicate that dermatological ultrasound operated by dermatologists who are experts in this technique, has high sensitivity as a diagnostic test for benign non-melanocytic cutaneous and subcutaneous skin tumors, which has an important application in daily clinical practice because it will help in decision-making when trying to avoid skin biopsies and unnecessary surgeries or scheduling them in a non-preferential way. That results in the consequent reduction of surgical waiting lists in health services and the improvement in the efficiency of such health systems, as well as a diminution of the possible surgical complications in patients such as surgical wound infections, wound dehiscence and the appearance of keloids that could be avoided, amongst others.
Ultrasound description of the primary criteria of high suspicion for benignity in non-melanocytic cutaneous and subcutaneous nodular tumors is determined by:
• Echogenicity of the tumor’s surrounding tissue-if it appears unaltered.
• Tumor’s size-if it is <5 mm.
• Tumor’s vascularization-if it is absent and/or scarce.
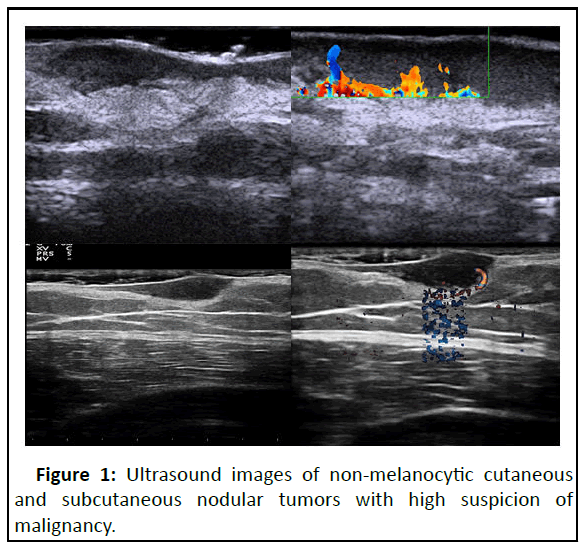
Ultrasound description of the primary criteria of high suspicion for malignancy in non-melanocytic cutaneous and subcutaneous nodular tumors is determined (Figure 1).
• Echogenicity of the tumor’s surrounding tissue-if it appears altered.
• Tumor’s size-if it is >5 mm.
• Tumor’s vascularization-if it is present and/or abundant.
The ultrasound description of the secondary criteria of high suspicion for benignity in nodular tumors would include the echogenicity of the lesion under study if homogeneous, it would be a factor in favor of a high suspicion for benignity and if, on the other hand, it is heterogeneous, this would have more risk of high suspicion for malignancy. Although this variable is nonsignificant when separated and isolated from others, it is useful so as to guide the diagnostic suspicion.
Conclusion
When ultrasound-analyzing and describing the nodule-tumor lesions, it is necessary to take into account not only the primary variables that are the reason for the study, but also the secondary ones described in 1) border (regular or irregular); 2) shape (round or oval); 3) morphology (lobed, multi-lobed); 4) location: Superficial (epidermis and superficial dermis) or deep (deep dermis and hypodermis); 5) echogenicity (homogeneous or heterogeneous); 6) posterior acoustic shadow (characteristic in hyperkeratotic lesions); 7) posterior reinforcement (characteristic in liquid-content lesions).
All these data plus those of the primary variables will help us improve our diagnostic judgment as dermatologists. Given these results, we can conclude that dermatological doppler ultrasound is a complementary and non-traumatic test that can be implemented in dermatology offices, whose use by experienced dermatologists entails a high diagnostic performance in benign non-melanocytic tumor lesions, as well as the screening of suspected malignant non-melanocytic tumor lesions.
Conflicts of Interest
Declarations of interest none.
Funding
This study has been funded by project PI16/00726 (Instituto de Salud Carlos III); and Fondo Europeo de Desarrollo Regional (FEDER) funds: "Una manera de hacer Europa”.
References
- Antoch J (2008) Environment for statistical computing. Comput Sci Rev 2: 113-122.
- Subirana I, Sanz H, Vila J (2014) Building bivariate tables: The compare groups package for R. J Stat Softw 57: 1-16.
- Annessi G, Bono R, Sampogna F, Faraggiana T, Abeni D (2007) Sensitivity, specificity and diagnostic accuracy of three dermoscopic algorithmic methods in the diagnosis of doubtful melanocytic lesions: The importance of light brown structureless areas in differentiating atypical melanocytic nevi from thin melanomas. J Am Acad Dermatol 56: 759-767.
[Crossref] [Google Scholar] [PubMed]
- Pralong P, Bathelier E, Dalle S, Poulalhon N, Debarbieux S, et al. (2012) Dermoscopy of lentigo maligna melanoma: Report of 125 cases. Br J Dermatol 167: 280-287.
[Crossref] [Google Scholar] [PubMed]
- Fonseca M, Marchetti MA, Chung E, Dusza SW, Burnett ME, et al (2015) Cross‐sectional analysis of the dermoscopic patterns and structures of melanocytic naevi on the back and legs of adolescents. Br J Dermatol 173: 1486-1493.
[Crossref] [Google Scholar] [PubMed]
- Avila-Tomas JF, Mayer-Pujadas MA, Quesada-Varela VJ (2021) Artificial intelligence and its applications in medicine II: Current importance and practical applications. Atencion Primaria 53: 81-88.
- Fornage BD, Tassin GB (1991) Sonographic appearances of superficial soft tissue lipomas. J Clin Ultrasound 19: 215-220.
[Crossref] [Google Scholar] [PubMed]
- Tsai WC, Chiou HJ, Chou YH, Wang HK, Chiou SY, et al. (2008) Differentiation between schwannomas and neurofibromas in the extremities and superficial body: The role of high‐resolution and color doppler ultrasonography. J Ultrasound Med 27: 161-166.
[Crossref] [Google Scholar] [PubMed]
- Jin W, Ryu KN, Kim GY, Kim HC, Lee JH, et al. (2008) Sonographic findings of ruptured epidermal inclusion cysts in superficial soft tissue: Emphasis on shapes, pericystic changes and pericystic vascularity. J Ultrasound Med 27: 171-176.
[Crossref] [Google Scholar] [PubMed]
- Zhong LP, Zhao SF, Chen GF, Ping FY (2004) Ultrasonographic appearance of lipoma in the oral and maxillofacial region. Oral Surg Oral Med 98: 738-740.
[Crossref] [Google Scholar] [PubMed]
- Kuwano Y, Ishizaki K, Watanabe R, Nanko H (2009) Efficacy of diagnostic ultrasonography of lipomas, epidermal cysts and ganglions. Arch Dermatol 145: 761-764.
[Crossref] [Google Scholar] [PubMed]
- Mentes O, Oysul A, Harlak A, Zeybek N, Kozak O, et al. (2009) Ultrasonography accurately evaluates the dimension and shape of the pilonidal sinus. Clinics 64: 189-192.
[Crossref] [Google Scholar] [PubMed]
- Wortsman X, Wortsman J (2010) Clinical usefulness of variable-frequency ultrasound in localized lesions of the skin. J Am Acad Dermatol 62: 247-256.
[Crossref] [Google Scholar] [PubMed]
- Wortsman X (2012) Common applications of dermatologic sonography. J Ultrasound Med 31: 97-111.
[Crossref] [Google Scholar] [PubMed]
- Llambias EJ, Bertotto GW, Risso C, Hernando I (2010) Quaternary volcanism in the Payenia retroarc: A review. Rev Assoc Geol Argentina 67: 278-300.
Open Access Journals
- Aquaculture & Veterinary Science
- Chemistry & Chemical Sciences
- Clinical Sciences
- Engineering
- General Science
- Genetics & Molecular Biology
- Health Care & Nursing
- Immunology & Microbiology
- Materials Science
- Mathematics & Physics
- Medical Sciences
- Neurology & Psychiatry
- Oncology & Cancer Science
- Pharmaceutical Sciences