Control of Hypertension at the Diabetic Outpatient Clinic of a National Referral Hospital, Uganda: A Cross Sectional Study
Mutebi Edrisa1, Birabwa Sserwanga Esther2*, Nakwagala Fredrick3, Muddu Martin3, Bagasha Peace3, Agaba Gideon3 and Kiggundu Daniel3
1Department of Medicine, Makerere University, Kampala, Uganda
2Department of Medicine, Centre for Diabetes Control, Kampala, Uganda
3Department of Medicine, Mulago National Referral Hospital, Kampala, Uganda
- *Corresponding Author:
- Birabwa Sserwanga Esther
Department of Medicine, Centre for Diabetes Control, Kampala, Uganda
E-mail: eflo87@yahoo.co.uk
Received date: Sep 17, 2020, Manuscript No. IPIBP-20-6164; Editor assigned date: Sep 22, 2020, PreQC No. IPIBP-20-6164(PQ); Reviewed date: Oct 06, 2020, QC No. IPIBP-20-6164; Revised date: June 28, 2022, QI No. Q-IPIBP-20-6164; Manuscript No. IPIBP-20-6164(R); Published date: July 26, 2022, DOI: 10.36648/2471-9897.8.4.26
Citation: Edrisa M, Esther BS, Fredrick N, Martin M, Peace B, et al. (2022) Control of Hypertension at the Diabetic Outpatient Clinic of a National Referral Hospital, Uganda: A Crosssectional Study. Insights Blood Press Vol.8 No.4:026
Abstract
Background: Non-Communicable Diseases (NCD’s) are globally becoming an epidemiological crisis because their burden continues to rise although they disproportionately affect the developing world especially the sub-Sahara African region. NCD’s are the leading cause of deaths and disability worldwide where about 46% of deaths in sub- Saharan Africa may be attributed to NCD’s by 2030. Hypertension (HT) and Diabetes Mellitus (DM) are the NCD’s of particular concern whose coexistence is a major contributor to the development and progression of macrovascular and microvascular complications.
HT is prevalent in 20%-60% of diabetics but conversely about 15% of hypertensive patients have concomitant diabetes and have an increased risk of developing diabetes than non-hypertensives, independent of any specific treatment. Hypertension is a major risk factor for mortality and CVD with 75% of cardiovascular disease in diabetic patients attributed to hypertension. Cardiovascular Disease (CVD) especially stroke accounts for almost 80% of deaths in diabetics but three-quarters of these occur in sub-Saharan Africa. Hypertension is among the most prevalent, modifiable cardiac risk factors for macrovascular disease in diabetic adults and therefore represents the most preventable cause of morbidity and premature mortality. Blood pressure control improves patient outcomes and reduces health care costs but is difficult within diabetics.
We aimed to estimate the prevalence of hypertension, explore hypertension control and investigate factors associated with poor hypertension control among patients attending the diabetic outpatient clinic at the national referral hospital in Uganda.
Methods: A cross-sectional study was conducted among 319 adult consenting patients attending the diabetic clinic of Mulago National Referral Hospital in Uganda between august and october 2018. Data was collected through interviewer administered questions using a standard pre tested questionnaire by trained staff.
Bivariate and multivariate logistic regression was performed to explore the association between factors and control of hypertension. The level of statistical significance was set at 95% confidence interval.
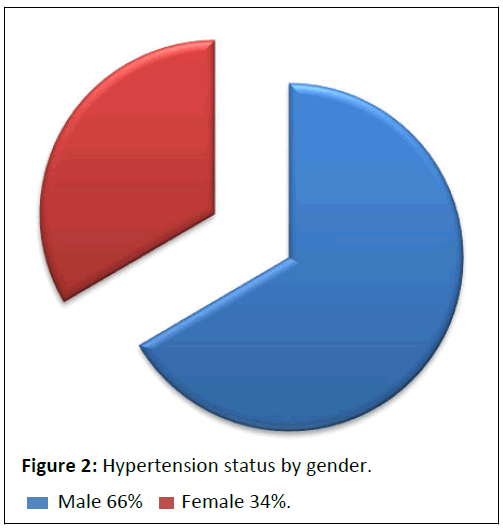
Results: Prevalence of hypertension noted was 88.09%, 25.27% were newly diagnosed with hypertension at the time of study data collection. Among those previously diagnosed/aware of their hypertension status, 130/210 (61.90%) were on hypertension treatment, 82% had their HT well controlled; 127 (60.48%) were on ACE and/or ARB. TG was independently associated with hypertension control in the multivariate analysis model (P=0.048).
Keywords
Hypertension prevalence; Hypertension control; Diabetes mellitus; Cross-sectional study
Abbreviations
ABI: Ankle Brachial Index; ACE inhibitors: Angiotensin Converting Enzyme inhibitors; BMI: Body Mass Index; BP: Blood Pressure; CAD: Coronary artery disease; CHD: Coronary heart disease; DBP: Diastolic Blood Pressure; HBAIC: Glycosylated Haemoglobin/haemoglobinA1c; HDL: High-Density Lipoprotein; LDL: Low-Density Lipoprotein; PAD: Peripheral Artery Disease; SBP: Systolic Blood Pressure; WHC: Waist Hip Circumference Ratio
Introduction
Non-Communicable Diseases (NCD’s) have become a global epidemiological crisis due to their escalating burden and they disproportionately affect the developing world especially the sub-Sahara African region. NCD’s are worldwide the leading cause of deaths and disability with an estimate of 46% of deaths in sub-Saharan Africa attributed to them by 2030 compared to about 28% in 2008. Demographic shifts such as increasing urbanization with associated lifestyle changes, changes in case ascertainment and diagnostic criteria, as well as improvements in life expectancy have contributed to a surge in NCD’s. Hypertension (HT) and Diabetes Mellitus (DM) are the NCD’s of particular concern in this epidemiological transition however, their precise epidemiological data are rare. In 2011, 366 million people were estimated with DM but projected to increase to 552 million by 2030 and there were about 422 million Diabetic adults world-wide in 2014. There is a global projection that diabetic adults will rise from 135 million in 1995 to 300 million in the year 2025 although most of this numerical increase will occur in developing countries. There will be more than 125 million Hypertensive adults in sub-Saharan Africa alone by 2025 which is the most experienced and reported NCD globally; in Uganda it is the most reported [1].
Research suggests that a strong association between hypertension and diabetes with the two often coexisting. HT is prevalent in 20%-60% of diabetics which is almost twice the frequency of hypertension in diabetic population as compared to age and gender-matched non-diabetic general population, but may range between 32% and 82% [2]. Hypertensives are more at risk of developing diabetes than non-hypertensives, independent of any specific treatment, about 15% of hypertensive patients have concomitant diabetes. Hypertension and diabetes mellitus have a complex cause-effect relationship, which is hypothesized [3].
The coexistence of hypertension and type 2 diabetes has supplementary effects and is a major contributor to the development and progression of macrovascular and microvascular complications which are often premature ones in diabetics compared to the general population [4]. The high burden of comorbid HT in diabetics together with an improvement in life expectancy in sub-Saharan Africa in the past 50 years results into complications and to experiencing the clinical syndromes of CVD since patients are exposed to hypertension risks for long periods. The presence of hypertension causes a 7.2-fold increase and a 37-fold increase in mortality in diabetic patients and indeed hypertension is the leading risk factor for mortality worldwide. Type 2 Diabetes Mellitus (DM) is a major cause of morbidity and death, primarily through its micro-vascular and macro-vascular complications [5].
Hypertension is a major risk factor for cardiac abnormalities, Cardiovascular Disease (CVD), stroke, myocardial infarction and ischaemic heart disease. Furthermore, up to 75% of cardiovascular disease in diabetics can be attributed to hypertension which further contributes to the overall morbidity and mortality of an already high risk population. CVD, especially stroke, accounts for up to 80% of all deaths in the diabetics and three-quarters of these deaths occur in sub-Saharan Africa [6]. Additionally, hypertension is a major causal factor of end-stage kidney failure, blindness and non-traumatic amputation in people with diabetes, where attributable risks are 50, 35 and 35% respectively. Diabetic Hypertensives are more likely to die when they develop complications. adequate hypertension control in diabetic hypertensives reduces the complication risks and is achieved through accurate, prompt and proper treatment although control of hypertension is difficult within diabetic patients [7].
Hypertension is among the most prevalent and modifiable cardiac risk factors for macro-vascular disease in adults with diabetes mellitus and therefore represents one of the most preventable causes of morbidity and premature mortality in developed as well as developing countries. Aggressive control of Blood Pressure (BP) improves patient outcomes and reduces health care costs but management of diabetic hypertensives also involves a multifactorial approach including lifestyle changes like dietary modifications, weight reduction, glycemic control, lipid management, increased physical activity, reduction in salt intake, tobacco cessation, appropriate sleep hygiene that are also known to improve metabolic health and reduce blood pressure however pharmacological interventions are frequently required to achieve optimal blood pressure goals in order to reduce mortality and cardiovascular events. All available treatment guidelines for these comorbidities from several professional societies also recommend achievement of similar goals in diabetics [8]. The National Kidney Foundation (NKF) hypertension and diabetes executive committees working group recommend lower blood pressure goals for Diabetics than for the general population. The most recent guidelines from the ADA and NKF recommend that blood pressure be decreased to less than 130/80 mm Hg, with an optimal target of below 120/80 mm Hg, especially in patients with proteinuria or renal insufficiency. The incidence of clinical complications among diabetics except for cataract extraction is significantly associated with systolic blood pressure and the lower the systolic blood pressure, the lower the risk of complications; each 10 mmHg decrease in mean systolic blood pressure is associated with risk reductions of 12% for any complication related to diabetes, 15% for deaths related to diabetes, 11% for myocardial infarction and 13% for microvascular complications [9].
Achieving the target BP of <130/85 mm Hg is the priority rather than the drug combination used in order to arrest and prevent the progression of complications in diabetic hypertensives. Regardless of the agents selected, a reduction in blood pressure helps to prevent and reduce diabetic complications with the lowest risk being in those with systolic blood pressure less than 120 mmHg [10]. In diabetic hypertensives, Angiotensin Converting Enzyme Inhibitors (ACEI’s) are the first line in management of hypertension but can be replaced by Angiotensin II Receptor Blockers (ARB’s) if patients are intolerant of them. There is an additional risk reduction with angiotensin converting enzyme inhibitors and β- blockers over and above that associated with lowering of blood pressure and adding both these agents may have beneficial effects on proteinuria. ACEI’s may provide additional benefits in patients with diabetes because they have also been shown to increase insulin sensitivity, β-blockers have been shown to reduce cardiovascular risk. In addition to lowering BP, it has been suggested that ARB’s reduce albuminuria which is a risk factor for progression to kidney disease and a surrogate marker for renal damage [11].
Unfortunately in sub-Saharan Africa awareness about the growing problem of NCD’s is low. In this study group, there is undiagnosed hypertension evidenced by the newly diagnosed who didn’t know that they had hypertension. Blood pressure control is poor among those on antihypertensive treatment and there is untreated disease among those with hypertension knowledge showing that the level of knowledge of the dangers of untreated hypertension in this population is low [12]. Undiagnosed, untreated and inadequate hypertension controls are significant risks of morbidity, complications and mortality for diabetic hypertensive patients. In addition to these issues the current guidelines for prevention and management of diabetes with hypertension in Uganda needs to be updated. There is therefore still need to explore hypertension control and associated factors among diabetics in Uganda [13].
Objectives
To estimate the prevalence of hypertension, explore the control of hypertension and investigate factors associated with poor control of hypertension among patients attending the diabetic outpatient clinic at Mulago national referral hospital in Uganda.
The findings will contribute to the guidelines on management of Diabetes Mellitus (DM) and hypertension in sub-Saharan Africa.
Methodology
This was a cross-sectional study that involved diabetic patients seeking care at the diabetic outpatient clinic of Mulago National Referral Hospital in Kampala, Uganda.
The duration of the study was 3 months between August and October 2018. Patients that presented to this clinic during the study period were enrolled after consenting in writing for study participation according to the inclusion criteria, but critically ill patients, newly diagnosed diabetes, those living more than 20 km from the clinic were excluded from the study. Enrolment was totally free and voluntary; participants were free to withdraw from the study at any time without any consequences to their future care at the clinic [14-17]. Approval to carry out the study was obtained from the ethics committee of the Uganda National Council of science and Technology, the School of Medicine research ethics committee of Makerere University College of Health Sciences.
Using a systematic sampling technique 319 study participants were recruited on the day that they came for their routine visits [18].
A predesigned, pre-tested structured questionnaire was used to collect information of study patients by trained health personnel on socio-demographic characteristics (age, gender, educational status, monthly income) physical activity which was involvement in physical exercises and the weekly exercises in hours, history about the duration of diabetes, family history of diabetes and Hypertension, drug history was taken. Body weight was measured using a weighing scale and was recorded to the nearest kilogram, height was measured in metres using a tape. All study subjects had their Blood Pressure (BP) measured using a sphygmomanometer in the right arm of the patient in sitting position [19,20].
The waist and hip circumference was recorded; BMI and the ABI were calculated; Body Mass Index (BMI) was obtained by dividing the weight in kilograms by the square of the height in meters. Blood Samples were taken for measurement of Random Blood sugar, HBAIC, HIV status, LDL, HDL, total glycerides and cholesterol. HbA 1c was measured using the mindray BS120 chemistry analyzer 2013-2006 by shenzhen mindray bio medical electronics Co [21].
Age was categorized as below and above 45 years, and educational status which was the highest level of education that the patient attained and reported during the interview was categorized as informal, formal, physical activity was a patients’ involvement in exercise and weekly exercises in hours was categorized as less or more than 4 hours per week while income was categorized as less or greater than 80 USD. BMI was classified into two categories (<25 and ≥ 25) with the normal as <25 kg/m2 and abnormal if >25 kg/m2. ABI was categorized into two categories as normal <1, abnormal if >1 [22].
Hypertension was defined as present if subjects had either a history of hypertension and/or evidence of hypertension (blood pressure ≥ 130/85 mmHg) [23,24].
Hypertension control was defined at a cut-off of Systolic Blood Pressure (SBP) 130 and/or Diastolic Blood Pressure (DBP) 85 mm of Hg among the patients that were aware of their hypertension status. Diabetic patients with previously diagnosed hypertension were considered to have uncontrolled hypertension if patients were on antihypertensive medications and the Systolic Blood Pressure (SBP) greater than or equal to 130 mm Hg and/or Diastolic Blood Pressure (DBP) greater than or equal to 85 mm Hg [25-28].
Data analysis
The data generated was entered, cleaned using epidata and analyzed using Stata statistical package: The patients’ records/ information was anonymised and de-identified prior to analysis.
Quantitative and qualitative statistical variables were crosstabulated; Bivariate and multivariate logistic regression was performed to explore the independent effect of factors and control of hypertension. All factors with p-value less than 0.2 in the bivariate model were entered into the multivariate model. Multivariate Logistic regression was performed where variables with a p-value less than 0.05 were considered as statistically significant predictors of hypertension. The level of statistical significance was set at 95% confidence interval [29,30].
Sample size estimation
The minimum required sample size was calculated to be 319 for this study using a sample size formula by Kish Leslie for crosssectional studies.
N=Z2 PQ/e2, Z=1.96
Where N=sample size estimate of adults with diabetes mellitus.
P=assumed true population disease prevalence, P=29.4%.
Q=the probability of not having DM=1-P=70.6%.
Z=Standard normal deviate at 95% confidence interval corresponding to 1.96.
e=precision=Absolute error between the estimated and true population disease prevalence of 5%.
The calculated sample size N=1.96 × 1.96 (0.294 × 0.706)/ 0.052=319.
Results
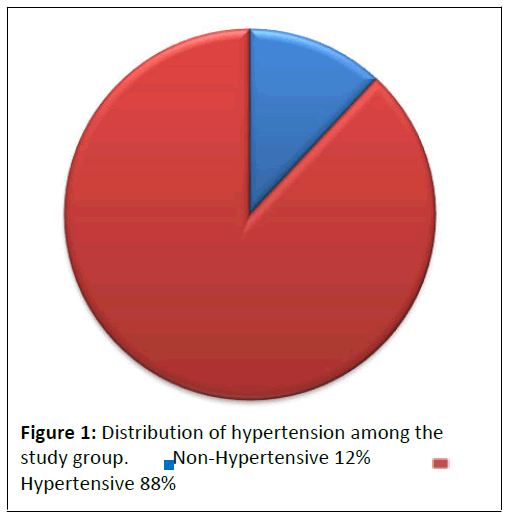
The study involved 319 participating patients who were predominantly female, 212 (66.46%) with their age range of 20 to 77 years with a mean age of 51.1 years [31-35].
99 (31.03%) patients were below 45 years old, 181 (56.74%) had informal education, 138 (43.26) had formal education up to tertiary level (Table 1).
| Variable | N (%) |
|---|---|
| Age | |
| below 45 | 99 (31.03) |
| above 45 | 220 (68.97) |
| Education | |
| Informal education | 181 (56.74) |
| Formal education | 138 (43.26 |
| Gender | |
| Male | 107 (33.54) |
| Female | 212 (66.46) |
| Income (dollars) | |
| Below $ 80 | 200 (62.70) |
| above $ 80 | 119 (37.30) |
| HIV | |
| Negative | 291 (91.22) |
| Positive | 28 (8.78) |
| History of HT | |
| Non-Hypertensive | 109 (34.17) |
| Hypertensive | 210 (65.85) |
| HBAIC | |
| Poor control | 195 (61.13) |
| Good control | 124 (38.87) |
| Duration of DM | |
| Below 10 yrs | 189 (59.25) |
| Above 10 yrs | 130 (40.75) |
| WHC ratio | |
| Abnormal | 50 (15.67) |
| Normal | 269 (84.33) |
| SBP | |
| Below 130 | 91 (28.53) |
| Above 130 | 228 (71.47) |
| DBP | |
| Below 85 | 146 (45.77) |
| Above 85 | 173 (54.23) |
| BMI | |
| Abnormal | 186 (58.31) |
| Normal | 133 (41.69) |
| ABI | |
| Abnormal | 29 (9.09) |
| Normal | 290 (90.91) |
| Family History of DM | |
| No | 127 (39.81) |
| Yes | 192 (60.19) |
| Family History of HT | |
| No | 116 (36.36) |
| Yes | 203 (63.64) |
| HDL | |
| Below 1.1 | 23 (7.21) |
| Above 1.1 | 296 (92.79) |
| LDL | |
| Below 2.6 (51.72) |
165 |
| Above 2.6 (48.28) |
154 |
| TCHOL | |
| Below 5.2 | 134 (42.01) |
| Above 5.2 | 185 (57.99) |
| TG | |
| Below 2.3 | 215 (67.40) |
| Above 2.3 | 104 (32.60) |
| Weekly Exercises | |
| Less than 4hrs | 127 (40.58) |
| More than 4hrs | 186 (59.42) |
| History of exercising | |
| No | 63 (19.75) |
| Yes | 256 (80.25) |
| History of Smoking | |
| No | 295 (92.48) |
| Yes | 24 (7.52) |
Table 1: Study population characteristics. Note: ABI: Ankle Brachial Index; BMI: Body Mass Index; DBP: Diastolic Blood Pressure; HBAIC: Glycosylated Haemoglobin/ haemoglobinA1c; HDL: High-Density Lipoprotein; LDL: Low- Density Lipoprotein; SBP: Systolic Blood Pressure; WHC: Waist Hip Circumference Ratio; TCHOL: Total cholesterol; TG: Triglyceride; DM: Diabetes mellitus; HT: Hypertension.
130 (40.75) had been suffering from diabetes for a period greater than 10 years. 195 (61.13%), had poor glycemic control, more than 50%, 186 (58.31%) of study participants had an abnormal BMI and 203 (63.64%) had a family history of hypertension (Table 1).
The prevalence of hypertension noted was 281/319 (88.09%)(Figure 1).
There were 186 (66.19%) females and 95 (33.81) males among those with Hypertension (Figure 2).
Among those who were Hypertensive, 71/281 (25.27%) were not aware of having hypertension at the time of the study from the history but were newly diagnosed with hypertension during study data collection. Among the patients that were aware of their hypertension status, 130/210 (61.90%) were on hypertension treatment [36].
In Table 2, we present the study population characteristics among those with known Hypertension status that were on treatment (Table 2).
| Variable | Poorly controlled | Well controlled | p-value |
|---|---|---|---|
| Age | |||
| below 45 | 9 (24.32) | 25 (14.45) | 0.139 |
| above 45 | 28 (75.68) | 148 (85.55) | |
| Education | |||
| Informal education | 21 (56.76) | 111 (64.16) | 0.397 |
| Formal education | 16 (43.24) | 62 (35.84) | |
| Gender | |||
| Male | 19 (51.35) | 50 (28.90) | 0.008 |
| Female | 18 (48.65) | 123 (71.10) | |
| Duration of DM | |||
| Below 10 yrs | 18 (48.65) | 96 (55.49) | 0.448 |
| Above 10 yrs | 19 (51.35) | 77 (44.51) | |
| HIV | |||
| Negative | 34 (91.89) | 157 (90.75) | 0.826 |
| Positive | 3 (8.11) | 16 (9.25) | |
| HBAIC | |||
| Abnormal | 22 (59.46) | 99 (57.23) | 0.803 |
| Normal | 15 (40.54) | 74 (42.77) | |
| WHC ratio | |||
| Abnormal | 9 (24.32) | 27 (15.61) | 0.202 |
| Normal | 28 (75.68) | 146 (84.39) | |
| Family History of HT | |||
| No | 15 (40.54) | 63 (36.42) | 0.637 |
| Yes | 22 (59.46) | 110 (63.58) | |
| Family History of DM | |||
| No | 15 (40.54) | 74 (42.77) | 0.803 |
| Yes | 22 (589.46) | 99 (57.23) | |
| BMI (kg/m2) | |||
| Abnormal | 21 (56.76) | 113 (64.20) | 0.394 |
| Normal | 16 (43.24) | 63 (3.80) | |
| ABI | |||
| Abnormal | 0 (0.00) | 20 (11.56) | 0.03 |
| Normal | 37 (100) | 153 (88.44) | |
| LDL | |||
| Below 2.6 | 25 (67.57) | 89 (51.45) | 0.074 |
| Above 2.6 | 12 (32.43) | 84 (48.55) | |
| HDL | |||
| Below 1.1 | 3 (8.11) | 10 (5.78) | 0.594 |
| Above 1.1 | 34 (91.89) | 163 (94.22) | |
| TG | |||
| Below 2.3 | 28 (75.68) | 105 (60.69) | 0.086 |
| Above 2.3 | 9 (24.32) | 68 (39.31) | |
| TCHOL | |||
| Below 5.2 | 19 (51.35) | 73 (42.20) | 0.308 |
| Above 5.2 | 18 (48.65) | 100 (57.80) | |
| ACE/ARB Use | |||
| No | 19 (51.35) | 64 (36.99) | 0.105 |
| Yes | 18 (48.65 | 109 (63.01) | |
| History of Exercising | |||
| No | 3 (8.11) | 27 (15.61) | 0.237 |
| Yes | 34 (91.89) | 146 (84.39) | |
| Weekly Exercises in hours | |||
| Less than 4 | 13 (35.14) | 65 (37.57) | 0.781 |
| More than 4 | 24 (64.86) | 108 (62.43) | |
| History of smoking | |||
| No | 34 (91.89) | 164 (94.80) | 0.489 |
| Yes | 3 (8.11) | 9 (5.20) | |
Table 2: Socio-Demographic characteristics by hypertension control among those with known history of status of hypertension. Note: ABI: Ankle Brachial Index; BMI: Body Mass Index; HBAIC: Glycosylated Haemoglobin/haemoglobinA1c; HDL: High-Density Lipoprotein; LDL: Low-Density Lipoprotein; WHC: Waist Hip Circumference Ratio; TCHOL: Total cholesterol; TG: Triglyceride; DM: Diabetes mellitus; HT: Hypertension; ACE inhibitors: Angiotensin Converting Enzyme inhibitors; HIV: Human immunodeficiency virus.
Among the patients with knowledge of Hypertension, 173/210 (82.38%) had their hypertension controlled. Good HT control was defined as a SBP less than 130 mm Hg and/or DBP less than 85 mm Hg among those on antihypertensive medication [37-39]. Use of either ARB or ACE was 60.48% among those who were aware of their Hypertension status.
Table 3 shows the relationship between HT control and predictive factors and only includes variables from bivariate analysis that had a significance at p<0.2. The following variables, Age, Gender, ACE/ARB use, WHC ratio, ABI, LDL and TG were associated with hypertension control in the bivariate model analysis and were the factors that were taken into the multivariate regression analysis.
| Hypertension Control | ||
|---|---|---|
| Test Statistic | ||
| Variables | P<(Z) | 95% conf. Interval |
| ACE/ARB use | 0.207 | -1.55 |
| Age | 0.159 | -1.87 |
| Gender | 0.144 | (-1.71)-(0 .25) |
| WHC ratio | 0.986 | -2.28 |
| LDL | 0.979 | (-0.30)-(0 .30) |
| TG | 0.048 | (0.01)-(0 .97) |
Table 3: Multivariate logistic regression analyses of factors associated with poor Hypertensive control in DM patients at the national referral hospital diabetic outpatient clinic, august to october 2018. Note: LDL: Low-Density Lipoprotein; WHC: Waist Hip Circumference Ratio; TG: Triglyceride; ACE inhibitors: Angiotensin Converting Enzyme inhibitors.
However TG was the only independent factor that showed significant association at p=0.048 with BP control in the multivariate model.
Discussion
Our study found that hypertension is a prevalent 88.09% comorbidity among diabetic patients at the specialized outpatient clinic of Mulago National Referral hospital which is in agreement with the statement that hypertension is a common problem for people with diabetes. Hypertension occurs more commonly in diabetics than in comparable non-diabetics [40,41]. This is in keeping with earlier studies, which found that the prevalence of hypertension in patients with diabetes was approximately twofold higher than in age-matched subjects without the disease and conversely, individuals with hypertension were at increased risk of developing diabetes compared with normotensive persons. This may be because both hypertension and DM patients have similar profiles. Previous observations suggest that demographic transition, urbanization and increasing life expectancy are major determinants of prevalence of hypertension among diabetics [42].
The rate of hypertension among diabetics in our study is comparable to the reported prevalence of hypertension in other studies in other populations, 74%, 74.4% and 73% rates of hypertension reported in UK Caucasians, Italian, and Spanish populations, respectively [43-47]. It is higher than the 82% prevalence rate reported about Afro-Caribbean individuals living in UK and much higher than the 32% and 39% rates reported among diabetics in the Turkish and Taiwanese populations, respectively. The prevalence of hypertension in a study among newly diagnosed diabetics was (62%) more than six patients out of 10 having hypertension. The rate reported is comparable in Arab populations of 64.5% and 72.4% reported in Qatari diabetics and Jordanian diabetics respectively but is however higher in other Arab populations of 53% in Saudi, 44% in Omani diabetics and 38% in Bahraini diabetics [48-55].
Unfortunately 71/281 (25.27%) of all those who are hypertensive in this study were not aware of having hypertension from the history but were newly diagnosed during the study and 210 (74.73%) knew their status. This is evident from other studies in the region, which found that the majority of patients with hypertension in sub-Saharan Africa did not know they were hypertensive and very few were on treatment, yet hypertension is the leading cause of stroke in Africa [56-60].
In another cross-sectional study in Uganda, awareness of hypertension was low, less than 30%. Furthermore, among those who knew they had hypertension, 130 (61.90%) were on treatment for hypertension [61-63]. This reflects the low level of knowledge of the dangers of untreated hypertension. In this population but carries a great risk for the complications of diabetes, especially CVDs such as stroke, LVH, myocardial infarction, as reported by the United Kingdom Prospective Diabetes Study (UKPDS) [64]. There is an additional risk reduction with Angiotensin Converting Enzyme inhibitors (ACE inhibitors) and β-blockers over and above that associated with lowering of blood pressure [65-70].
The results of this study also show that HT control is not adequate in this diabetic study population, 173/210 (82.38%) had their hypertension controlled. This finding is consistent with what other studies that reported a proportion of hypertensive patients with DM with inadequate control of BP [71].
Patient factors contribute to poor blood pressure control through non adherence to medications and follow-up visits. Health care costs may reduce adherence by some patients. Inadequate patient knowledge about hypertension and CVD risk is likely to be an additional contributor [72,73]. In a 2002 survey, nearly two-thirds of people with diabetes did not consider CVD to be a common complication of diabetes, more than half did not consider themselves personally at risk for CVD and only 5% recognized that reducing blood pressure could lower CVD risk. Blood pressure control is the lynchpin of cardiovascular risk reduction, its optimal control may be even more important in diabetic patients, yet, copious research demonstrates that a high proportion of hypertensive patients do not achieve blood pressure control that conforms to current recommendations.
There was suboptimal control in the majority, >70%, of nondiabetic and diabetic patients even in the context of high (91%) adherence to prescribed regimens, less than 10% in a crosssectional study and in another retrospective study conducted in an urban diabetes clinic in Kampala, 56% of the patients had optimal blood pressure control, defined as ≤ 140/80 mmHg [74,75]. This confirms earlier conclusions in Uganda that blood pressure control among adult diabetic patients is sub-optimal. The possible explanation for the low level of HT control noted in our study could be that the majority of people with hypertension are not aware they have the condition, and even among those who are aware, less than half are receiving treatment. This may be due to the patient’s underestimation of the potential complications of hypertension, non-compliance, absence of effective health education programs, low level of education and/or low socioeconomic levels [76]. However, even among those receiving treatment, eighty three in one hundred have optimally controlled blood pressure. The low levels of Hypertension control are a worrying global trend that is widespread in both low- and high-income countries. 56.74% of study participants had informal education (primary level and below). Illiteracy is usually associated with low income, unemployment which may contribute to the high frequency of hypertension because anti-hypertensives are daily medications whose costs may be high and unaffordable to these patients [77].
While new data caution against excessive BP and glucose control in certain subpopulations, studies continue to suggest that appropriate lowering of BP in diabetes is important for improving macrovascular outcomes. Each 10 mmHg decrease in updated mean systolic blood pressure is associated with risk reductions of 12% for any complication related to diabetes, 15% for deaths related to diabetes, 11% for myocardial infarction and 13% for microvascular complications [78].
Age, gender, ACE/ARB use, WHC ratio, ABI, LDL and TG were associated with hypertension control in the bivariate model. Among these factors, Ankle Brachial Index (ABI), LDL and TGL are modifiable, while gender is the non-modifiable factor associated with hypertension control. However in the multivariate model only TG was independently associated with hypertension control in this model. Mounting evidence indicates that elevated triglyceride level is a risk factor for Coronary Heart Disease (CHD) and that high triglyceride levels are associated with several risk factors including suboptimal BP control that substantially increase the risk of CAD [79,80].
The results of this study show that Hypertension (HT) is common among this Diabetic clinic’s patients and that HT control in DM is not adequate.
Conclusion
The prevalence of Hypertension among diabetic patients at this diabetic clinic in Uganda was high. Quite a number of these patients were not aware of their HT status and even among those aware that they were hypertensive, some were not on HT treatment.
Hypertension control is sub-optimal even among those with known hypertension status and on anti-hypertensive medication. This requires clear national guidelines to be put in place on the management of hypertension in Diabetic patients.
Ethics Statement
Approval to carry out the study was obtained from the Institutional Review Board (IRB) of the Uganda National Council of science and Technology, the School of Medicine research ethics committee of Makerere University College of Health Sciences. Written informed consent was obtained from patients to participate in this study after a comprehensive explanation of the purpose and procedure of the study.
Data Sharing Statement
The datasets used and/or analyzed during the current study are available from the corresponding author on request.
Disclosure
The authors report no conflicts of interest in this work.
Funding
The study was Nurture fellowship under the grant Number D43TW10132 supported by Office of The Director, National Institutes of Health (NIH), National Institute of Dental and Craniofacial Research (NIDCR), National Institute of Neurological Disorders and Stroke (NNDS), National Heart, Lung and Blood Institute (NHLB), Forgarty International Centre (FIC), National Institute on Minority Health and Health Disparities (NIMHD).
Authors’ Contributions
I contributed in conceiving the idea, study design, drafting, data analysis, interpretation, managing the overall progress of the study and write up of the manuscript. BSE was involved in study design, data analysis, writing up and editing of the manuscript. The others equally contributed in data analysis, drafting and in revising the manuscript. The final manuscript was read and approved by all the authors.
Acknowledgements
I would like to acknowledge the Nurture fellowship under the grant number D43TW10132 supported by Office of The Director, National Institutes of Health (NIH), National Institute of Dental and Craniofacial Research (NIDCR), National Institute of Neurological Disorders and Stroke (NNDS), National Heart, Lung And Blood Institute (NHLB), Forgarty International Centre (FIC), National Institute On Minority Health and Health Disparities (NIMHD).
Authors are very grateful for the study participants, data collectors and supervisors.
References
- Kavishe B, Biraro S, Baisley K, Vanobberghen F, Kapiga S, et al. (2015) High prevalence of hypertension and of risk factors for Non-Communicable Diseases (NCDs): A population based cross-sectional survey of NCDS and HIV infection in Northwestern Tanzania and Southern Uganda. BMC Med 13: 1-21.
- Kotwani P, Kwarisiima D, Clark TD, Kabami J, Geng EH, et al. (2013) Epidemiology and awareness of hypertension in a rural Ugandan community: a cross-sectional study. BMC Pub Health 13: 1-10.
- Musinguzi G, Nuwaha F (2013) Prevalence, awareness and control of hypertension in Uganda. PloS One 8: e62236.
- King H, Aubert RE, Herman WH (1998) Global burden of diabetes, 1995-2025: prevalence, numerical estimates, and projections. Diabetes care 21: 1414-1431.
- Twagirumukiza M, De Bacquer D, Kips JG, de Backer G, Vander Stichele R, et al. (2011) Current and projected prevalence of arterial hypertension in sub-Saharan Africa by sex, age and habitat: an estimate from population studies. J Hypertens 29: 1243-1252.
- Bloomfield GS, Barasa FA, Doll JA, Velazquez EJ (2013) Heart failure in sub-Saharan Africa. Curr Cardiol Rev 9: 157-173.
- Moran AE, Tzong KY, Forouzanfar MH, Roth GA, Mensah GA, et al. (2014) Variations in ischemic heart disease burden by age, country, and income: The global burden of diseases, injuries, and risk factors 2010 study. Glob Heart 9: 91-99.
- Whiting DR, Guariguata L, Weil C, Shaw J (2011) IDF diabetes atlas: global estimates of the prevalence of diabetes for 2011 and 2030. Diabetes Res Clin Pract 94: 311-321.
- WHO: WHO Global report on diabetes 2016 WHO/NMH/NVI/16.3.
- King H, Aubert RE, Herman WH (1998) Global burden of diabetes, 1995-2025: prevalence, numerical estimates, and projections. Diabetes Care 21: 1414-1431.
- Wild S, Roglic G, Green A, Sicree R, King H (2000) Global prevalence of diabetes. Estimates for 2000 and projections for 2030. Diabetes Care 27: 104753.
- Maher D, Waswa L, Baisley K, Karabarinde A, Unwin N (2011) Epidemiology of hypertension in low-income countries: A cross-sectional population-based survey in rural Uganda. J Hypertens 29: 1061-1068.
- Maher D, Waswa L, Baisley K, Karabarinde A, Unwin N, et al. (2011) Distribution of hyperglycaemia and related cardiovascular disease risk factors in low-income countries: A cross-sectional population-based survey in rural Uganda. Int J Epidemiol 40: 160-171.
- Mondo CK, Otim MA, Akol G, Musoke Robert, Orem J (2013) The prevalence and distribution of non-communicable diseases and their risk factors in Kasese district, Uganda: cardiovascular topics. Cardiovasc J Afr 24: 52-57.
- Paul B, Sapra B, Maheshwari S, Goyal RK (2000) Role of losartan therapy in the management of diabetic hypertension. J Assoc Physicians India 48: 514-518.
- Sowers JR, Haffner S (2002) Treatment of cardiovascular and renal risk factors in the diabetic hypertensive. Hypertension 40: 781-788.
- Tarnow L, Rossing P, Gall MA, Nielsen FS, Parving HH (1994) Prevalence of arterial hypertension in diabetic patients before and after the JNC-V. Diabetes Care 17: 1247-1251.
- Satman I, Yilmaz T, Sengul A, Salman S, Salman F, et al. (2002) Population-based study of diabetes and risk characteristics in Turkey: results of the Turkish Diabetes Epidemiology study (TURDEP). Diabetes Care 25: 1551-1556.
- Tseng CH (2006) Higher risk of hypertension in indigenous type 2 diabetic patients in Taiwan. J Hyperten 24: 1817-1821.
- Baskar V, Kamalakannan D, Holland MR, Singh BM (2002) The prevalence of hypertension and utilization of antihypertensive therapy in a district diabetes population. Diabetes Care 25: 2107-2108.
- Comaschi M (2005) SFIDA Study Group-Italian Association of Diabetologists (AMD): Cardiovascular risk factors and metabolic control in type 2 diabetic subjects attending outpatient clinics in Italy: the SFIDA (survey of risk factors in Italian diabetic subjects by AMD) study. Nutr Metab Cardiovasc Dis 15: 204-211.
- del Cañizo-Gómez FJ, Moreira-Andrés MN (2004) Cardiovascular risk factors in patients with type 2 diabetes: Do we follow the guidelines?. Diabetes Res Clin Pract 65: 125-133.
- Baskar V, Kamalakannan D, Holland MR, Singh BM (2006) Does ethnic origin have an independent impact on hypertension and diabetic complications?. Diabetes Obes Metab 8: 214-219.
- Robert Lee Page II: Morning hypertension and diabetes: powerful predictor for future complications: hypertension in patients with diabetes pharmacy times 2008-11-01 05:00:00.
- Weycker D, Nichols GA, O'Keeffe-Rosetti M, Edelsberg J, Khan ZM, et al. (2007) Risk-factor clustering and cardiovascular disease risk in hypertensive patients. Am J Hypertens 20: 599-607.
- (1994) National high blood pressure education program working group report on hypertension in diabetes. Hypertension 23: 145-58.
[Crossref][Google Scholar][Indexing]
- Libby P, Nathan DM, Abraham K, Brunzell JD, Fradkin JE, et al. (2005) Report of the national heart, lung, and blood institute-national institute of diabetes and digestive and kidney diseases working group on cardiovascular complications of type 1 diabetes mellitus. Circulation 111: 3489-3493.
- Fong DS, Aiello LP, Ferris FL, Klein R (2004) Diabetic retinopathy. Diabetes Care 27: 2540-53.
- Tesfaye S, Chaturvedi N, Eaton SE, Ward JD, Manes C, et al. (2005) Vascular risk factors and diabetic neuropathy. N Engl J Med 352: 341-350.
- Sowers JR, Williams M, Epstein M, Bakris G (2000) Hypertension in patients with diabetes: strategies for drug therapy to reduce complications. Postgrad Med 107: 47-60.
- Kengne AP, Amoah AG, Mbanya JC (2005) Cardiovascular complications of diabetes mellitus in sub-Saharan Africa. Circulation 112: 3592-3601.
- Cowie CC, Rust KF, Byrd-Holt DD, Eberhardt MS, Flegal KM, et al. (2006) Prevalence of diabetes and impaired fasting glucose in adults in the US population: National Health And Nutrition Examination Survey 1999-2002. Diabetes Care 29: 1263-1268.
- Collins AJ, Kasiske B, Herzog C, Chen SC, Everson S, et al. (2001) Preface: Excerpts from the United States renal data system 2001 annual data report: Atlas of end-stage renal disease in the United States. Am J Kidney Dis 38.
- Molitch Mark E, Defronzo Ralph A, Franz Marion J, Keane William F, Mogensen Carl Erik (2002) American diabetes association. diabetic nephropathy. Diabetes Care 25: S85-9.
- Lawes CM, Vander Hoorn S, Rodgers A (2008) Global burden of blood-pressure-related disease, 2001. Lancet 371: 1513-1518.
- Yach D, Hawkes C, Gould CL, Hofman KJ (2004) The global burden of chronic diseases: overcoming impediments to prevention and control. Jama 291: 2616-2622.
- Lim SS, Vos T, Flaxman AD, Danaei G, Shibuya K, et al. (2012) A comparative risk assessment of burden of disease and injury attributable to 67 risk factors and risk factor clusters in 21 regions, 1990-2010: A systematic analysis for the global burden of disease study 2010. Lancet 380: 2224-2260.
- Diabetes control and complications trial research group (1993) The effect of intensive treatment of diabetes on the development and progression of long-term complications in insulin-dependent diabetes mellitus. N Engl J Med 329: 977-986.
- UK prospective diabetes study group (1998) Tight blood pressure control and risk of macrovascular and microvascular complications in type 2 diabetes. Bmj 317: 703-713.
- Schrier RW, Estacio RO, Esler A, Mehler P (2002) Effects of aggressive blood pressure control in normotensive type 2 diabetic patients on albuminuria, retinopathy and strokes. Kidney Int 61: 1086-1097.
- King P, Peacock I, Donnelly R (1999) The UK prospective diabetes study (UKPDS): clinical and therapeutic implications for type 2 diabetes. Br J Clin Pharmacol 48: 643.
- Cooper R, Rotimi C, Ataman S, McGee D, Osotimehin B, et al. (1997) The prevalence of hypertension in seven populations of West African origin. Am J Public Health 87: 160-168.
- Berraho M, El Achhab Y, Benslimane A, Rhazi KE, Chikri M, et al. (2012) Hypertension and type 2 diabetes: A cross-sectional study in Morocco (EPIDIAM Study). Pan Afr Med J 11.
- Sowers JR (2003) Recommendations for special populations: diabetes mellitus and the metabolic syndrome. Am J Hypertens 16: 41S-45S.
- Sowers JR, Epstein M, Frohlich ED (2001) Diabetes, hypertension, and cardiovascular disease: an update. Hypertension 37: 1053-1059.
- Adler AI, Stratton IM, Neil HAW, Yudkin JS, Matthews DR, et al. (2000) Association of systolic blood pressure with macrovascular and microvascular complications of type 2 diabetes (UKPDS 36): prospective observational study. BMJ 321: 412-419.
- Makowsky M, Prebtani AP, Gelfer M, Manohar A, Jones C (2012) Management of hypertension in people with diabetes mellitus: translating the 2012 Canadian hypertension education program recommendations into practice. Can J Diabetes 36: 345-353.
[Crossref][Google Scholar][Indexing]
- Dinh W, Lankisch M, Nickl W, Scheyer D, Scheffold T, et al. (2010) Insulin resistance and glycemic abnormalities are associated with deterioration of left ventricular diastolic function: A cross-sectional study. Cardiovasc Diabetol 9: 1-12.
- Konzem SL, DeVore VS, Bauer DW (2002) Controlling hypertension in patients with diabetes. Am Fam Physician 66: 1209.
- Casas JP, Chua W, Loukogeorgakis S, Vallance P, Smeeth L, et al. (2005) Effect of inhibitors of the renin-angiotensin system and other antihypertensive drugs on renal outcomes: systematic review and meta-analysis. Lancet 366: 2026-2033.
- Furberg CD, Wright JT, Davis BR, Cutler JA, Alderman M, et al. (2002) Major outcomes in high-risk hypertensive patients randomized to angiotensin-converting enzyme inhibitor or calcium channel blocker vs diuretic: The Antihypertensive and Lipid-Lowering Treatment to Prevent Heart Attack Trial (ALLHAT). JAMA 288: 2981-2997.
- Centers for disease control and prevention, National center for chronic disease prevention and health promotion. National diabetes statistics report, 2014. Estimates of diabetes and its burden in the United States, 2017.
- Stults B, Jones RE (2006) Management of hypertension in diabetes. Diabetes Spectr 19: 25-31.
[Crossref][Google Scholar][Indexing]
- Gæde P, Lund-Andersen H, Parving HH, Pedersen O (2008) Effect of a multifactorial intervention on mortality in type 2 diabetes. N Engl J Med 358: 580-591.
- Gæde P, Vedel P, Larsen N, Jensen GV, Parving HH, et al. (2003) Multifactorial intervention and cardiovascular disease in patients with type 2 diabetes. New Engl J Med 348: 383-393.
- American Diabetes Association (2002) Standards of medical care for patients with diabetes mellitus. Diabetes Care 25: s33-s49.
- Bakris GL (2000) National kidney foundation hypertension and diabetes executive committees working group. Preserving renal function in adults with hypertension and diabetes: A consensus approach. Am J Kidney Dis 36: 646-661.
- UK Prospective Diabetes Study Group (1998) Efficacy of atenolol and captopril in reducing risk of macrovascular and microvascular complications in type 2 diabetes: UKPDS 39. BMJ 317: 713-720.
- Cutler JA (1996) High blood pressure and end-organ damage. J Hypertens Suppl 14: S3-6.
- Tuomilehto J, Rastenyte D, Birkenhäger WH, Thijs L, Antikainen R, et al. (1999) Effects of calcium-channel blockade in older patients with diabetes and systolic hypertension. N Engl J Med 340: 677-684.
- Muddu M, Mutebi E, Ssinabulya I, Kizito S, Mondo CK (2018) Hypertension among newly diagnosed diabetic patients at Mulago National Referral Hospital in Uganda: a cross sectional study. Cardiovasc J Afr 29: 218-224.
- Bener A, Zirie M, Janahi IM, Al-Hamaq AO, Musallam M, et al. (2009) Prevalence of diagnosed and undiagnosed diabetes mellitus and its risk factors in a population-based study of Qatar. Diabetes Res Clin Pract 84: 99-106.
- Mubarak FM, Froelicher ES, Jaddou HY, Ajlouni KM (2008) Hypertension among 1000 patients with type 2 diabetes attending a national diabetes center in Jordan. Ann Saudi Med 28: 346-351.
- Akbar DH, Ahmed MM, Algambi AA (2003) Cardiovascular risk factors in Saudi and non-Saudi diabetics. Saudi Med J 24: 686-687.
- Al-Moosa S, Allin S, Jemiai N, Al-Lawati J, Mossialos E (2006) Diabetes and urbanization in the Omani population: An analysis of national survey data. Popul Health Metr 4: 1-8.
- Al-Mahroos F, Al-Roomi K, McKeigue PM (2000) Relation of high blood pressure to glucose intolerance, plasma lipids and educational status in an Arabian Gulf population. Int J Epidemiol 29: 71-76.
- BeLue R, Oluwole AN, Degboe AN, Figaro MK (2012) Hypertension control in ambulatory care patients with diabetes. Am J Manag Care 18: 17-23.
- Merz CNB, Buse JB, Tuncer D, Twillman GB (2002) Physician attitudes and practices and patient awareness of the cardiovascular complications of diabetes. J Am Coll Cardiol 40: 1877-1881.
- Okonofua EC, Simpson KN, Jesri A, Rehman SU, Durkalski VL, et al. (2006) Therapeutic inertia is an impediment to achieving the Healthy People 2010 blood pressure control goals. Hypertension 47: 345-351.
- Saaddine JB, Cadwell B, Gregg EW, Engelgau MM, Vinicor F, et al. (2006) Improvements in diabetes processes of care and intermediate outcomes: United States, 1988-2002. Ann Intern Med 144: 465-474.
- Chelminski P, Pignone M (2008) The quandary of improving hypertension control in diabetes. Clin Diabetes 26: 158-160.
- Kibirige D, Atuhe D, Sebunya R, Mwebaze R (2014) Suboptimal glycaemic and blood pressure control and screening for diabetic complications in adult ambulatory diabetic patients in Uganda: A retrospective study from a developing country. J Diabetes Metab Disord 13: 1-7.
- Pereira M, Lunet N, Azevedo A, Barros H (2009) Differences in prevalence, awareness, treatment and control of hypertension between developing and developed countries. J Hypertens 27: 963-975.
- Psaltopoulou T, Orfanos P, Naska A, Lenas D, Trichopoulos D, et al. (2004) Prevalence, awareness, treatment and control of hypertension in a general population sample of 26 913 adults in the Greek EPIC study. Int J Epidemiol 33: 1345-1352.
- Dzudie A, Kengne AP, Muna WF, Ba H, Menanga A, et al. (2012) Prevalence, awareness, treatment and control of hypertension in a self-selected sub-Saharan African urban population: A cross-sectional study. BMJ Open 2: e001217.
- Advance collaborative group (2008) Intensive blood glucose control and vascular outcomes in patients with type 2 diabetes. New Eng J Medicine 358: 2560-2572.
- Riddle MC (2010) Effects of intensive glucose lowering in the management of patients with type 2 diabetes mellitus in the action to control cardiovascular risk in diabetes (ACCORD) trial. Circulation 122: 844-846.
- Accord study group (2010) Effects of intensive blood-pressure control in type 2 diabetes mellitus. New Eng J Med 362: 1575-1585.
- Hokanson JE (2002) Hypertriglyceridemia and risk of coronary heart disease. Curr Cardiol Rep 4: 488-493.
- Coughlan BJ, Sorrentino MJ (2000) Does hypertriglyceridemia increase risk for CAD? Growing evidence suggests it plays a role. Postgrad Med 108: 77.
Open Access Journals
- Aquaculture & Veterinary Science
- Chemistry & Chemical Sciences
- Clinical Sciences
- Engineering
- General Science
- Genetics & Molecular Biology
- Health Care & Nursing
- Immunology & Microbiology
- Materials Science
- Mathematics & Physics
- Medical Sciences
- Neurology & Psychiatry
- Oncology & Cancer Science
- Pharmaceutical Sciences
 Non-Hypertensive 12%
Non-Hypertensive 12%  Hypertensive 88%
Hypertensive 88%